Understanding Schizophrenia
Lesson 14
Schizophrenia
Derived from the Greek 'schizo' (splitting) and 'phren' (mind or soul)
Dr Emile Kreplin was the first doctor, back in the year 1887. He then used the term Dementia Praecox to describe anyone who suffered from the symptoms aligned to the condition, we recognize now as schizophrenia.
Nonetheless, Paul Eugen Bleuler, in 1908, during a lecture of the German Psychiatric Association in Berlin, then coined the term schizophrenia being based on his previous studies on psychiatric patients in Europe to be a functional psychotic disorder who had difficulty relating to the world.
He then characterized this further by the presence of, delusional beliefs, hallucinations, and disturbances in their thought perception, and behaviour.
At that meeting, Professor Bleuler argued that dementia praecox was associated with neither dementia nor precociousness and emphasized that splitting of the mind being, an essential feature of schizophrenia.
One of the most striking differences between Emil Kraepelin and Bleuler is that Kraepelin collected information about his patients from their documents. Whereas, Bleuler collected this information through careful clinical observations.
Recover From Schizophrenia

Schizophrenia affects around 1% of the population, the National Alliance to End Homelessness reports that people with schizophrenia make up to 20% of the homeless population.
Individuals with schizophrenia experience anosognosia, which is the lack of awareness of the severity of their condition.
There is currently no cure for the illness, but there are enough treatments and therapies available for suffers to be able to find a form of medication and talking therapy (Psychotherapy) — The goal of therapy is to help you learn about the illness, establish goals and manage everyday problems related to the disorder.
It also can help you manage the feelings of distress associated with the symptoms and challenge thoughts that might not be based on reality. Helping them to live a full and healthy life. It used to be thought of as a “hopeless” condition, but improvements in the way it can be handled mean that it can be much easier to cope with than it was 100 years ago.
Causes of schizophrenia
The exact cause of schizophrenia is unknown. But most experts believe the condition is caused by a combination of genetic and environmental factors. Individuals who have relatives with schizophrenia tend to have a higher risk of developing it. It's thought that some people are more vulnerable to developing schizophrenia, and certain situations can trigger the condition, such as a stressful life event or drug misuse.
Schizophrenia is a highly heritable genetic disorder
Research has shown that heredity or genetics can be an important contributing factor for the development of schizophrenia. While there is no one clear-cut cause for the condition, a genetic gene mutation of neurotransmitters in the brain is impaired in patients with schizophrenia, known to predispose people to a range of neurodevelopmental disorders.
Although a single-gene mutation can put people at risk for schizophrenia, autism, Tourette syndrome and other neuropsychiatric disorders, there are 30 schizophrenia-associated loci that have been identified but “at the end of the day, we still don’t know what causes schizophrenia.
A 2017 study from Denmark based on nationwide data on over 30,000 twins estimates the heritability of schizophrenia at 79 per cent.

Biochemical pathway into schizophrenia
There is one common association that schizophrenia patients have and that is the fact they will all have raised levels of the chemical dopamine in their brains. Dopamine is a “feel good” chemical that we all need to keep our moods stable. If it drops too low we are likely to suffer from depression, low mood and anxiety. If it is raised too high, we can end up suffering from delusions and/or hallucinations.
While, antipsychotic drugs are thought to exert their main therapeutic effects by blocking the dopamine receptor.
Along with genetics, other potential causes of schizophrenia include:
- The environment. Being exposed to viruses or toxins, or experiencing malnutrition before birth, can increase the risk of schizophrenia.
- Brain chemistry. Issues with brain chemicals, such as the neurotransmitters dopamine and glutamate, may contribute to schizophrenia.
- Substance use. Teen and young adult use of mind-altering (psychoactive or psychotropic) drugs may increase the risk of schizophrenia.
- Immune system activation. Schizophrenia can also be connected to autoimmune diseases or inflammation.
Archives of Schizophrenia throughout History
Schizophrenia was widely considered by then to be a fully functioning mental illness affecting around 1%, of the population worldwide and is associated with substantial morbidity and mortality. However, if we look back in time, we learn it has existed much earlier and was recorded in a holy Egyptian papyrus text called The Book of Hearts, and it is in there that we find the earliest mentions of psychotic disorders such as schizophrenia.
Records from Hindu descriptions in Atharvana Veda date back to 1400 BC. Vedas are acknowledged to be the backbones of Hinduism. Within these writings, it has been assumed, that health is the outcome of equilibrium between five elements (Bhuthas) and three humours (Doshas) and that any disproportion between these elements might result in mental illness.
How is schizophrenia diagnosed?

If symptoms are present, your doctor will perform a complete medical history and physical examination. Although there are no laboratory tests to specifically diagnose schizophrenia, the doctor might use various diagnostic tests such as MRI or CT scans or blood tests to rule out physical illness as the cause of your symptoms.
Early symptoms
Symptoms of this disorder commonly show up in the teenage years and early 20s. At these ages, the earliest signs may get overlooked because of typical adolescent behaviours.
Positive symptoms
“Positive” symptoms of schizophrenia are behaviours that aren't typical in otherwise healthy individuals. These behaviours include:
Hallucinations
Are experiences that appear real but are created by your mind.
They include seeing things, hearing voices, or smelling things others around you don't experience.
Delusions.
A delusion occurs when you believe something despite evidence or facts to the contrary.
Thought disorders.
These are unusual ways of thinking or processing information.
Movement disorders.
These include agitated body movements or strange postures
Negative symptoms
Negative symptoms of schizophrenia interrupt a person's typical emotions, behaviours, and abilities. These symptoms include:
Disorganized thinking or speech, where the person changes topics rapidly when speaking or uses made-up words or phrases
Trouble controlling impulses
Odd emotional responses to situations
A lack of emotion or expressions
Loss of interest or excitement for life
Social isolation
Trouble experiencing pleasure
Difficulty beginning or following through with plans
Difficulty completing everyday activities
Cognitive symptoms
Cognitive symptoms of schizophrenia are sometimes subtle and may be difficult to detect. However, the disorder can affect memory and thinking.
These symptoms include:
disorganized thinking, such as trouble focusing or paying attention
poor “executive functioning,” or understanding information and using it to make decisions
problems learning information and using it
lack of insight or being unaware of their symptoms
Symptoms of schizophrenia can be difficult to detect.
Psychosocial intervention
The doctor or therapist then determines if the person's symptoms point to a specific disorder as outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which is published by the American Psychiatric Association and is the standard reference book for recognized mental illnesses. According to the DSM-5, to be diagnosed with schizophrenia, two or more of the following must be present during 1 month. At least one must be numbers 1, 2, or 3 on the list:
- Delusions
- Hallucinations
- Disorganised speech
- Grossly disorganised or catatonic behaviour
- Negative symptoms (diminished emotional expression or motivation)
Alternative treatments for schizophrenia
Medication is important for treating schizophrenia. However, some individuals with the disorder may want to consider complementary medicine.
If you choose to use these alternative treatments, work with your doctor to make sure the treatment is safe.
Types of alternative treatments used for schizophrenia include:
- vitamin treatment
- fish oil supplements
- glycine supplements
- diet management
Research supporting these alternative treatments is limited.
Schizophrenia spectrum Disorder (SSD)
Schizophrenia is a spectrum disorder under which many other disorders fall, including but not limited to schizotypal personality disorder, schizoaffective disorder, schizophreniform disorder, and schizophrenia.
Psychotic symptoms
These are experiences similar to those experienced in schizophrenia, including:
- Hallucinations - where you may experience things that others around you don't. For example hearing voices, seeing visual hallucinations and other unexplained sensations.
- Delusions - where you might hold strong beliefs that other people don't share. For instance, a fear that you are being followed, your thoughts are being read, you are very powerful and able to influence things outside your control, or that you have special insight or divine experiences.
The main symptoms of schizophrenia include hallucinating, experiencing delusions, and/or disorganised speech/behaviour.
To qualify for a diagnosis of schizophrenia, one must have two of the above-listed symptoms, along with a lowered ability to function in daily life.
Medication — The primary medications used to treat psychotic symptoms — such as delusions, hallucinations and disordered thinking — are called antipsychotics. A group of newer medicines, called atypical antipsychotics, are most commonly used.
These include:
It’s important to educate yourself and your family to help them cope with your illness and detect early signs of relapse.
Paranoid schizophrenia
Paranoid schizophrenia was the most commonly diagnosed form of the disorder. Then, in 2013, the American Psychiatric Association decided schizophrenia subtypes weren't separate conditions.
Today, a doctor or healthcare professional won't diagnose someone with this condition.
The diagnosis instead will be simply schizophrenia. The predominant symptom may be paranoia, though. Knowing this will help inform a doctor about potential treatment plans.
Not everyone with the disorder will experience paranoia. However, recognizing the symptoms of paranoid schizophrenia can help you or a loved one get treatment.
Catatonic schizophrenia
Catatonic was another previously used type of schizophrenia. However, it's no longer used as a diagnosis. Instead, only one type is then diagnosed.
The symptoms of catatonic schizophrenia included:
Schizophrenia vs. psychosis
Psychosis may be confused for one another, but they're not the same. One is a mental health condition, the other is a symptom.
Psychosis is a break from reality. During an episode of psychosis, you may hear voices, see things that aren't real, or believe things that aren't true.
Psychosis is one element or symptom of several mental health disorders, including schizophrenia. Psychosis can also occur in people with no other symptoms of mental health issues.
Although psychosis can occur in people with schizophrenia, not everyone with this disorder will experience psychosis. If you or someone you know is experiencing symptoms of psychosis, seek treatment immediately.
Schizoaffective disorder is a condition where symptoms of both psychotic and mood disorders are present together during one episode (or within two weeks of each other).
The word schizoaffective has two parts:
- ‘schizo–‘ refers to psychotic symptoms
- ‘–affective’ refers to mood symptoms.
You might have times when you struggle to look after yourself, or when your doctors consider that you lack insight into your behaviour and how you are feeling.
Schizoaffective differs only in the way that a mood disorder must also be present, and an individual must first and foremost be struggling with depression, mania, and/or hypomania.
Is schizoaffective disorder similar to schizophrenia or bipolar?
Schizoaffective disorder is its own diagnosis. However, when someone is experiencing both psychotic and mood symptoms at the same time, it can be difficult to determine what they are experiencing and how best to understand and classify these experiences.
Schizoaffective with Bipolar can be Bipolar Type 1 or Type 2
This is often mistaken, with Bipolar with Psychotic Features. Schizoaffective with Bipolar is when psychosis symptoms stay consistent for the most part between depression, hypomania, and mania episodes. If psychosis is only happening when manic, then, it is not Schizoaffective.
Schizotypal personality disorders (SPD)
Schizotypal personality disorder can affects 4% of the general population in the United States.
Like schizophrenia and other psychotic disorders, the schizophreniform disorder is a type of mental illness — called a “psychosis” — in which you cannot tell what is real from what is imagined.
Although schizophrenia is a lifelong illness, schizophreniform disorder lasts between one and six months. About one person in 1,000 develops schizophreniform disorder during his or her lifetime. The disorder occurs equally in men and women between the ages of 18 and 24. However, it often strikes men at a younger age. In women, it most often occurs between the ages of 24 and 35.
About two-thirds of people with the schizophreniform disorder develop schizophrenia. In some cases, people with the schizophreniform disorder also have symptoms of depression, which increases the risk of suicide.

Schizophrenia complications
Doctors often describe schizophrenia as a type of psychosis. This means the person may not always be able to distinguish their own thoughts and ideas from reality.
According to the Royal College of Psychiatrists, 3 out of every 5 people diagnosed with schizophrenia will get better with treatment.
To get on the road to improvement, it's important to:
- learn about your condition
- understand the risk factors
- Following your doctor's recommendations will improve your prognosis. (healthline.com)
Schizophrenia has both positive and negative symptoms. Positive symptoms are those that affect the individual’s thoughts or behaviours.
They include:
- delusions
- hallucinations
- strange or inexplicable behavioural changes
- confusion or thought disorder
People with schizophrenia may experience one or more of these symptoms.
Hallucinations
Many people with schizophrenia do not realize that they are unwell. Hallucinations and delusions can seem very realistic to a person who is experiencing them. This can make it hard to convince the individual to take medication. They may fear the side effects or believe that the medication will harm them.
Schizophrenia usually appears when a person is in their late teens or older, but it can also affect children.
Some people experience hallucinations. The most common type is hearing voices, but hallucinations can affect all the senses. For example, a person may also see, feel, taste, or smell things that are not really there.
Delusions
A delusion is something that a person believes without a doubt to be true, despite evidence to the contrary. These delusions, which are typically based on something false or unrealistic, often cause the individual to act differently than usual. They may even try to use a delusional idea to justify or explain their actions.
An individual who experiences delusions may believe that there are hidden messages in common, everyday occurrences. They may find a meaning that does not really exist in, for example, the colour of someone’s clothes or a media broadcast.
A person with schizophrenia may also have the feeling that someone is watching or following them, or talking about them behind their back. As a result, they may become suspicious of close friends or family members. This is sometimes known as “paranoid schizophrenia,” and it occurs in nearly 50% of individuals with the condition. Various environmental and genetic factors may trigger paranoid schizophrenia.
Delusions may continue for several weeks or even months. According to a slightly older 20-year study that followed 200 individuals with schizophrenia, 57% of people experienced recurring delusions during the study.
Confused thinking and speech
A person’s thinking, and speech, may jump from one subject to another for no logical reason. It may therefore be hard to follow what the person is trying to say.
There may also be memory problems and difficulty understanding and using information.
Behavioural and thought changes
People with schizophrenia often experience unpredictable changes in behaviour or thought. They believe that another entity is partially or fully controlling them, either in mind or body or both.
Thought disorder
Thought disorder is a confused, disorganized way of thinking that may result in a person expressing themselves in unusual ways when speaking or writing. It is common in schizophrenia and other psychotic disorders.
Thought disorder relates to a person’s ability to sustain concentration and focus, evaluate situations in a logical and coherent fashion, and plan and execute tasks in a goal-directed and logical way. Both behaviour and language can be indicators of a thought disorder.
Famous People Who had Schizophrenia
It can make it difficult to work and even function due to symptoms of hallucinations, delusions, disorganized speech, social withdrawal and other behaviours, according to WebMD.
Nevertheless, there are many famous people who have had the condition. One of the most notable currently is Brian Wilson, who came to fame in The Beach Boys.
It is alleged he suffered from the condition during a period of self-destructive living in the late 1970s and 1980s, during which time he became addicted to drugs and also started to suffer from compulsive overeating.
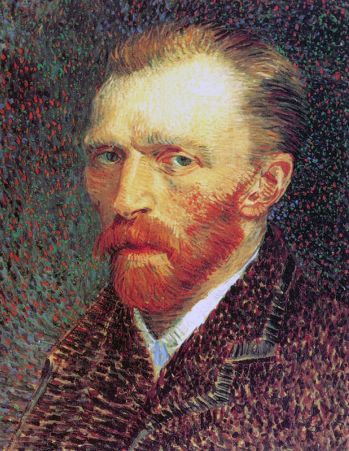
It is argued by some that painter Vincent van Gogh had the condition, though his symptoms also drew parallels with bipolar disorder.
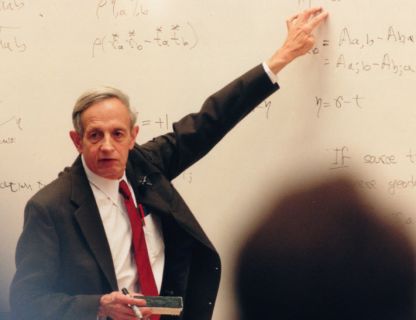
If you’ve seen or read “A Beautiful Mind” by Sylvia Nasar, you know who this man is. John Forbes Nash Jr., who died in 2015.
He was a prolific mathematician and economist, earning a Nobel Prize for the latter in 1994 for his work on game theory along with two other theorists.
In the book, Nasar profiles his lifelong battle with schizophrenia.
Eleanor Longden
You may recognize Eleanor Longden from her TED Talk, “The Voices in My Head,” which has garnered more than five million views.
She currently works as a postdoctoral researcher at the Psychosis Research Unit at the University of Manchester.
She draws on her own experience with schizophrenia and psychosis to advocate for more holistic approaches for treating auditory hallucinations and other symptoms of psychosis.
Eleanor Longden
You may recognize Eleanor Longden from her TED Talk, “The Voices in My Head,” which has garnered more than five million views. She currently works as a postdoctoral researcher at the Psychosis Research Unit at the University of Manchester. She draws on her own experience with schizophrenia and psychosis to advocate for more holistic approaches for treating auditory hallucinations and other symptoms of psychosis.
Elyn Saks
Elyn Saks in her, “A Tale of Mental Illness,” or her memoir, “The Center Cannot Hold My Journey Through Madness.” She is an esteemed university professor at the University of Southern California where she advocates for better mental health laws.
Her schizophrenia did not stop her from holding an impressive academic track record at Vanderbilt, Oxford and Yale, where she earned her law degree.
Elyn Saks won the MacArthur’s Genius Grant in 2009 for her memoir. Her activism weaves closely with her professionalism in that her other works include advocating for the rights of people with mental illness.
Though she struggled with many hospitalizations over the years, she found success in her career and love life and resides in California with her husband.
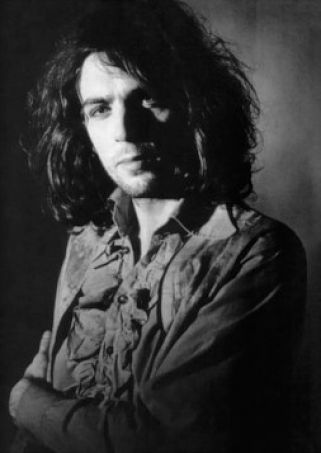
Syd Barrett, a co-founder of Pink Floyd, had schizophrenia
Schizophrenia, has affected the lives of many public figures. While known to have died from diabetes complications at the age of 60, Syd Barrett seems to have had schizophrenia, too.
The condition was likely to have links to his genetics. It is possible that stressful childhood and career contributed as well.
All of that might have triggered the abuse of psychedelic drugs, (LSD) in his twenties.
Here are 4 myths about schizophrenia, it’s time to bust
It’s time to bust these myths about living with schizophrenia.
People don’t really know what schizophrenia is.
Myth 1: People with schizophrenia are violent and dangerous.
Schizophrenia is not insane, psycho, crazy, mad, dangerous, violent.
From 1990-2010, 41 movies had a character with schizophrenia that engaged in violent behaviour.
But in reality, a person with schizophrenia is more likely to be a victim of a crime than to commit one.
The condition affects men and women equally, though women tend to develop it later in life, due to hormone fluctuations. Statistically, schizophrenia sufferers are less likely to engage in violent behaviour than people without the condition.
Myth 2: People with schizophrenia have multiple personalities.
One of the first questions the Human Resources person asked was: “So do you think you’re two people?” And no, schizophrenia is not a multiple personality disorder.
Myth 3: Hallucinations go away as soon as the medication is taken.
Medication can help, but it doesn’t mean all the symptoms just go away.
Still, people with schizophrenia can live full, productive lives even while “hearing voices.”
Myth 4: Hallucinations are the only symptoms.
People with schizophrenia can also experience delusions, social withdrawal, and blurred emotional responses.
These disorders can also give you a very poor ability to focus because your thoughts are so disorganized. Your thoughts are so fast. They’re racing in your head. And it’s kind of a mental overload. You just can’t focus on the outside world.
https://themighty.com/video/4-myths-about-schizophrenia-its-time-to-bust/
People with schizophrenia deserve to be understood. It’s time we start listening to them.
Calling anyone with a mental disorder insane, psycho, crazy or mad is insulting. And it’s almost always incorrect.
Finally, Facts about Schizophrenia
facts and stats 1. People living with schizophrenia smoke cigarettes up to three times more.
That has led scientists to believe that nicotine is a form of self-medication among schizophrenia patients. Interestingly, nicotine can help normalize specific deficits in the central nervous system. That explains the higher rate of smokers among people with schizophrenia compared to people with other mental conditions.
facts and stats 2. Around 50% of individuals living with schizophrenia have a history of substance abuse.
Schizophrenia patients often turn to illegal substances for self-medication.
They also turn to those to alleviate some symptoms or co-occurring psychological disorders. Based on addiction and schizophrenia data, marijuana, cocaine, and alcohol are some of the most used substances.
facts and stats 3. Schizophrenia symptoms fall into three categories.
Symptoms can be positive, such as hallucinations and delusions, or negative. The latter are the symptoms that disrupt normal behaviour. Those include feeling no pleasure, problems speaking, and difficulty starting or finishing activities. The third category is the cognitive symptoms. These affect a person’s way of thinking. Such symptoms range from memory issues and trouble focusing to difficulties in the decision-making process.
facts and stats 4. There are four different types of schizophrenia.
This disorder exhibits different symptoms for everyone. However, there are four major categories into which patients generally fall:
- Paranoid schizophrenia. Facts show its main characteristics — paranoia, suspicion, and fear of other people’s intentions.
- Catatonic schizophrenia. It causes people to shut down physically, as well as emotionally and mentally.
- Undifferentiated schizophrenia. It displays different symptoms, like confusion, paranoia, or abnormal behaviour.
- Schizoaffective disorder. Delusions and hallucinations might come hand in hand with at least one symptom of a mood disorder, such as depression and mania.
facts and stats 5. 23% of people with schizophrenia also have OCD.
It’s very common for people with schizophrenia to have other, co-occurring mental health issues. Thus, 15% of people with schizophrenia have panic disorder, while 29% have PTSD.
What’s more, between 30% and 54% of schizophrenia patients display symptoms of depression.
facts and stats 6. Schizophrenia affects between 150,000 and 200,000 Australians.
The rate of incidence of schizophrenia in Australia is relatively high.
That said, the government is diligent about creating different strategies.
Those strategies aim to improve mental health treatment and services.
As a result, many mental health programs have emerged in recent years.
facts and stats 7. Around 1.2% of Americans have this disorder, schizophrenia statistics for the US report.
That translates to about 3.2 million American adults who have schizophrenia. That said, it’s difficult to determine the exact number of individuals living with schizophrenia in America.
That is mostly because of its complexity and because it overlaps with other conditions.
Namely, it might overlap with substance abuse, bipolar disorder, and multiple personality disorder.
facts and stats 8. Schizophrenia statistics by state show that California has the most adults with this condition.
With 335,242 adults diagnosed with schizophrenia, California has the highest incidence. The 2017 Census data also shows that Texas is second with 230,324 cases and Florida comes third with 184,607. On the other hand, Wyoming has the lowest prevalence rate of schizophrenia — only 4,871 cases in 2017. Sadly, 1,948 of those cases were untreated.
facts and stats 9. Around 20 million people in the world have schizophrenia.
To begin with, schizophrenia has direct links to cognitive, perceptive, and emotional disruptions. The main symptoms are hallucinations, delusions, and disorganized behaviour (or speech). Another symptom is emotional disturbances.
In other words, there is a disconnection between the emotions reported and corresponding body language.
facts and stats 10. Adolescents might be the turning point for schizophrenia.
Statistics show that it’s very uncommon to develop symptoms of schizophrenia before the age of 12 or after 40.
In fact, the average age of schizophrenia onset is that of late teens or early 20s.
Scientists are not entirely sure why this is the case, but they believe it might be due to a combination of genetics, brain changes, and hormones.
facts and stats 11. In 40% of patients with schizophrenia or schizoaffective disorder are left-handed.
Scientists agree that left-handedness can have links to creative skills in different fields. They also speculate that creative individuals are more likely to have schizophrenia. It is also possible for them to have a schizoaffective disorder.
facts and stats 12. The prevalence rate of schizophrenia among children under 13 is about 1 in 10,000.
Childhood-onset schizophrenia is rare and tends to be more common among boys.
Diagnosing COS still incites controversy among healthcare professionals.
That is because most of the symptoms overlap with other conditions.
Namely, children with autism also experience hallucinations and delusions.
What’s more, psychosis is not uncommon with mood disorders, such as depression and anxiety.
facts and stats 13. Black people are three to four times more likely to be diagnosed with psychotic disorders.
Race, ethnicity, and religion may not make you vulnerable to the disorder. That said, the data on the prevalence of schizophrenia by race show racial disparities.
Those become more evident when it comes to diagnosing mental disorders.
Not only are Blacks more commonly diagnosed with psychotic disorders, but they’re also more likely to receive a misdiagnosis.
A recent study revealed concerning information.
Astoundingly, clinicians tend to factor in racial bias when diagnosing schizophrenia.
facts and stats14. Genetic variations increase your risk by 80%, according to schizophrenia stats and facts.
Although there isn’t just one factor listed among schizophrenia causes, studies reveal that genetic variation plays a considerable role.
In fact, one research discovered that chances of having the disorder increase by 10% if a parent or a sibling has it.
If both parents have it, then there is a 40% chance that their child will have schizophrenia, too. Still, the greatest risk is if an identical twin has it.
In that case, the other twin has a 50% chance of having schizophrenia.
facts and stats 15. Certain mind-altering drugs put users at higher risk of schizophrenia.
Drugs like methamphetamines or LSD can make the occurrence of schizophrenia more likely. Cannabis use might pose a similar risk, marijuana and schizophrenia facts reveal.
One research shows that the younger the individuals are when they start using drugs, the more likely they are to experience symptoms.
Those symptoms include delusions, hallucinations, and cognitive dysfunction.
facts and stats 16. Fish oil could reduce the risk of developing the condition.
Fish oil, a rich source of omega-3 acids, can reduce inflammation in the body and aid brain development and function.
According to the data on the prevalence of schizophrenia, a lack of these fatty acids can have links to the disorder.
This discovery prompted scientists to carry out a study on 81 young people at risk of schizophrenia.
The study confirmed that those who took fish oil supplements were less likely to develop the condition.
facts and stats 17. People with schizophrenia die at a younger age.
According to schizophrenia statistics in the US, the average potential life loss for people with this condition is 28.5 years. Heart disease, diabetes, and liver disease contribute to early mortality rates.
Lack of proper nutrition, physical activity, and social stigma also affect the quality of life and leads to premature death.
facts and stats 18. Around 5% to 6% of schizophrenia patients die by suicide.
Furthermore, about 20% of people with schizophrenia attempt suicide at least once in their life.
The schizophrenia suicide rate is much higher than that of the general population.
Notably, young males are more at risk of attempting or committing suicide.
The more common symptoms of the illness, hallucinations and delusions, do not seem to be responsible for the high rate of suicide.
What does contribute to suicidality is hopelessness, social stigma, and unemployment?
facts and stats 19. Total (direct and indirect) costs of schizophrenia amount to nearly $63 million a year.
Despite the low prevalence rates of schizophrenia, this is quite a costly disease. Its overall cost includes direct and indirect expenses.
First, direct costs are counselling and medication.
Second, indirect expenses are lost productivity and financial assistance.
Both can reach up to $63 million per year.
Furthermore, this disorder contributes 13.4 million YLDs to the global burden of the disease, or 1.7% of total YLDs in 2016.
facts and stats 20. Most Common Schizophrenia Facts vs. Misconceptions
Schizophrenia is one of the most commonly misunderstood mental disorders. Many people don’t have a clear idea of what this condition entails.
That leads to numerous misconceptions and social prejudice.
facts and stats 21. People with schizophrenia don’t have “multiple personalities.”
One of the most common schizophrenia facts and myths is that people with the disorder have split personalities. In fact, 64% of Americans believe that the conditions have a lot in common when, in reality, they don’t.
People with schizophrenia can lose touch with reality and sometimes act like two different people. However, that is not the same as having a multiple personality disorder.
facts and stats 22. Schizophrenia and violence statistics break the link between the two.
A recent study involving 1,435 participants showed acts of violence to be quite rare. In fact, 19 out of 20 participants didn’t report any violence during the 2-year follow-up period.
The study also looked into the participants who had been victims of violence.
Those people were more likely to exhibit violent behaviour.
facts and stats 23. Schizophrenia facts point to many creative and overall brilliant people who had the disorder.
Even though some people with schizophrenia have problems with attention, memory, and focus, it doesn’t mean that they’re not smart. Actually, there have been many creative and famous people with schizophrenia.
These include an artist Vincent van Gogh, a Nobel Prize-winning mathematician John Nash, and a novelist Jack Kerouac.
facts and stats 24. There is no cure for schizophrenia.
Even though there isn’t a cure for this disorder, schizophrenia is still a treatable and manageable disease. Taking antipsychotic schizophrenia medication is one of the essential steps.
That said, it shouldn’t be the only method of treatment.
A combination of community support, healthy and balanced nutrition, and self-care are just as important.
facts and stats 25. Interesting facts about schizophrenia show that high doses of vitamin B can reduce the symptoms.
A review found out that high doses of B vitamins, such as B6, B8, and vitamin B12, effectively reduce the symptoms of psychosis.
The study also discovered that B-vitamins could reduce residual symptoms.
That said, we need more studies to prove their efficacy.
facts and stats 26. Nutrition also plays a crucial role in schizophrenia treatment and could lower the rate of schizophrenia.
There are quite a few things one could do when it comes to balancing the disorder. For starters, balancing blood sugar, increasing the amount of essential fats, and following a healthy diet may work wonders. Vitamin C supplements, folic acid, and zinc supplements are also much-needed nutrients.
facts and stats 27. In 20% of people with schizophrenia will recover within five years from experiencing the first symptoms.
What percentage of people with the disorder recover?
Unfortunately, schizophrenia is a life-long disease.
What’s more, recovery doesn’t mean that challenges will completely disappear.
However, people can still learn to manage their symptoms.
Schizophrenia statistics show that 80% will continue to remain chronically ill and require daily support throughout their lives.
facts and stats 28. Based on schizophrenia recovery rates, 99% of individuals with schizophrenia need lifelong treatment.
Almost all people diagnosed with the disorder need medication, counseling, and social rehabilitation throughout their lives.
Antipsychotics, such as Chlorpromazine or Clozapine, are usually administered.
However, depending on the condition and the severity of the symptoms, other medications can also be prescribed.
facts and stats 29. Nonadherence rates range from 26.5% to 58.8% of the population.
People living with schizophrenia consistently show low adherence to their medication.
That could affect the development of the disease and the rate of schizophrenia hospitalization, statistics show.
According to one study, the most common reason for not taking the medication is a lack of awareness.
In fact, 55% of respondents stated that they don’t take medication because they don’t believe they’re sick.
facts and stats 30. Over 69% of individuals with schizophrenia don’t get the care they need.
One of the reasons why most people with schizophrenia do not get proper treatment is social stigma.
Facts about schizophrenia report that feeling stigmatized makes them less likely to seek medical care.
What’s more, 90% of people with untreated schizophrenia live in low- and middle-income countries.
That translates to the lack of access to adequate mental health care.
facts and stats 31. Around 70% of people with schizophrenia experience hallucinations
(https://www.goodtherapy.org/learn-about-therapy/issues/schizophrenia/statistics)
As a paper just published in Frontiers in Psychology points out, congenital and early blindness appears to protect against schizophrenia. As the authors note, “across all past papers, there has not been even one reported case of a congenitally blind person who developed schizophrenia.” However, this is not so with blindness developed later in life.
The authors conclude that it must be brain changes that occur secondarily to congenital and early blindness—not blindness itself—that protect against schizophrenia. They then go on to give an account of what those changes may be.
But the authors also point out that autism is very common in blind children by contrast to both congenital deafness and deaf-blindness, which are associated with increased risk of psychosis. Indeed, an earlier study confirmed previous ones in finding that “there are blind children who do not satisfy the diagnostic criteria for autism, but who nevertheless have marked impairments in interpersonal engagement," adding that "These are the very same children who also manifest several additional ‘autistic features.’”
Another additional autistic feature—albeit a comparatively rare one—is savantism, and here it may be worth pointing out that the combination of blindness, autism, and musical genius is unusually frequent. (The classic case is Blind Tom and his living equivalent is Leslie Lemke, as I explain in The Imprinted Brain).
Furthermore, the cognitive, sensory, and neurological factors that are cited as contributing protection against schizophrenia in the Frontiers in Psychology paper are frequently found in people with autism. The very first one the authors mention—pitch discrimination—is a case in point.
Some estimate that up to a third of all people with autism have perfect pitch, and enhanced sensitivity to sound is widely reported in autism.
Sense of smell is also superior in autism: In one study by Tavassoli and others due to appear in Autism, an autistic group proved able to detect a test odour at a mean distance of almost twice that of normal controls. The study also found a quantitative relationship between levels of enhanced sensory processing and the number of autistic traits, with greater severity of autistic behaviour related to higher sensory perception.
Although mentalistic deficits combined with mechanistic and sensory compensations seem to be a primary developmental factor in autism, they are probably a secondary consequence of the loss of sight in blind individuals. For example, gaze-monitoring is one of the key factors in mentalism (or mind-reading skills) because it conveys so much information about what a person is thinking, feeling, or intending. Indeed, deficits here are one of the earliest and most reliable indicators of autism. Obviously, this skill is totally lacking in the blind, whose mind-reading abilities must be correspondingly compromised by their incapacity to monitor gaze.
But such mentalistic deficits might be compensated for through greater sensitivity in other senses, such as touch, which certainly substitutes for vision in reading Brail, and is generally enhanced in the congenitally blind. But studies also show a lower threshold of sensitivity to touch in people with autism as compared to non-autistic controls. Indeed, there is evidence that enhanced sensitivity to touch and to sound are correlated in autism.
Vision has also been found to be strikingly enhanced in some people with high-functioning autism, whose acuity is on a level with that of birds of prey (almost three times better than average). And although there is obviously no direct parallel with congenital blindness here, the authors of the Frontiers of Psychology study point out that the congenitally blind are protected from the abnormal visual inputs which have been implicated in schizophrenia.
Furthermore, the visual cortex in congenitally blind people is thicker than in the sighted, but as the authors point out this thickening “is thought to be characterized by a less than normal amount of pruning, due to deprivation of visual experience.” Schizophrenics, by contrast, have a thinner cortex.
In previous posts, I have drawn attention to both proliferation of neurons in the frontal brain and of dendrites in those with autism, who typically are born with bigger brains and thicker cortices than normal.
And as I also pointed out, brain development is more like sculpture than building: neurons are pruned to produce the end result, not incrementally added. So the lack of such pruning may be another feature common to both autism and congenital blindness.
Finally, the authors point out that “it has already been demonstrated in schizophrenia that improving auditory precision by repeated practising of tone discrimination leads to improvements in auditory and (more interestingly) higher-level cognitive functions.” Indeed, they even mention “fostering cognitive reserve” as a corrective to what I would call the hyper-mentalism of schizophrenia.
The imprinted brain theory’s diametric model of mental illness proposes that autism is the mentalistic opposite of psychoses such as schizophrenia. Put very crudely, the diametric model suggests that the best way to cure psychotics is to make them somewhat autistic, and pitch-discrimination training in particular and fostering cognitive reserve, in general, are examples of how this can be done, as I pointed out in an earlier post.
Indeed, anything that can push the balance in the autistic direction will suffice to counter psychotic tendencies, and early-onset blindness certainly appears to do so where providing protection from schizophrenia is concerned—just as the diametric model predicts.