- in News by Tony
- |
- 1 comments
COVID-19 outbreak.
What Is COVID-19?
The novel coronavirus set in motion a global pandemic that the world is still attempting to understand, treat and grapple with.
The virus is a novel member of the coronavirus family of viruses, long associated with the common cold, SARS (Severe Acute Respiratory Syndrome), and MERS (Middle East Respiratory Syndrome). The virus is believed to have existed in animals before recently mutating and undergoing transmission to humans.
More...
The world we currently live in has become a very strange and turbulent place. Coronavirus has transformed everything we thought we knew about our daily lives, our government, and our health into a kind of bizarro world where FaceTime dating and panic-buying toilet paper are the new norm.
It’s taking a toll on even the most optimistic of us as we try to stay positive amidst what feels like bleaker and bleaker news each day. Now, imagine how this already unsettling situation feels for the over 45 million Americans with mental illness.
Those suffering from anxiety, depression, PTS, substance abuse, and other forms of chronic mental illness are some of the most vulnerable right now in terms of loneliness, isolation, and potential for self-destructive behavior due to a lack of consistent support and a disrupted routine.
In an effort to help those with mental illness (and their friends and loved ones who may be concerned about the impacts COVID-19 may be having on them), we spoke to the experts on the specific challenges those with the most common conditions face, as well as what actions they can practice and networks they can access to remain healthy and safe.
Because it is a new virus, its behaviour, its virulence, its means of spread, and other essential features are only now under study. Infectious disease experts around the world are providing valuable information about the virus almost daily that can help curb its spread.
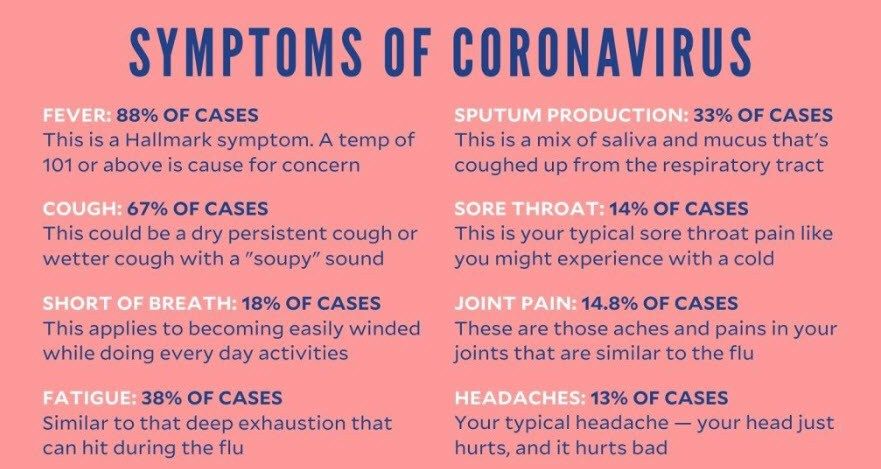
The virus leads to an illness called Coronavirus Disease 2019 or COVID-19. People with the disease typically have a fever, cough, trouble breathing, and exhaustion.
Coronavirus presents as an upper respiratory illness with symptoms similar to pneumonia. You can become symptomatic anywhere from two to fourteen days after exposure. It is a highly contagious disease that can be spread from person-to-person contact.
Respiratory droplets that are released in the air when someone infected coughs or sneezes, and possibly by touching a surface or object with the virus on it and then touching your mouth, nose, or eyes. However, the CDC does not consider that last one is a primary way the virus is transmitted.
Most people who get the disease recover on their own with no lasting consequences, according to the World Health Organization. But up to 20 per cent of cases may need urgent medical attention. Those most at risk include elderly adults and people with underlying health conditions.
Men appear to experience at least twice the risk of complications and death as women, and obesity as well as diabetes, heart disease, and immunologic conditions are reported risk factors for serious illness. Because the virus has a particular affinity for lung tissue, breathing can become compromised, and patients requiring hospital care often need the assistance of a mechanical ventilator or respirator.
Simple actions like washing your hands, not touching your face, and staying home when sick can help keep everyone safe. Social distancing and avoiding large gatherings are also vital to curbing transmission.
What Are The Dangers For Those With Chronic Mental Illness?
If you feel nervous or scared about the current situation, multiply that by 1000 and you’ll begin to understand how this situation feels to those suffering from mood and personality disorders.
The novelty of the coronavirus threat, the uncertainty about its behaviour, and the necessary adoption of restrictive measures to contain its spread, such as social isolation, have created unusual conditions giving rise to unprecedented levels of anxiety.
The effects of this crisis are more far-reaching than heightened anxiety, which pretty much everyone is feeling. There are also trickle-down effects to those with addiction and behavioral disorders like OCD, ADHD, and substance abuse.
Along with the good that social distancing can do for our own health and society in general, it also increases feelings of isolation, loneliness, stress, and fear—all of which can be triggers that make many mental illnesses infinitely worse.
Anxiety is an unpleasant sensation that generally serves as a stimulus to take appropriate action. Still, the very measures taken to curb the coronavirus require that people refrain from most forms of activity. As a result, the impact of anxiety is magnified, and many people feel helpless.
Social isolation is a severe psychological and physiological stressor, and the stress of separation is likely to hit hardest those people who, for one reason or another, are already devoting significant energy and resources to adapt to everyday life.
These include, but are not limited to, the socially anxious, the unemployed, those with pre-existing mental health problems, those at risk for domestic violence and child abuse, older people coping with hearing or eyesight problems, and those experiencing cognitive decline.
Managing Anxiety and Fear

As governments, corporations, and individuals work to contain the spread of the virus, it is natural to experience stress or fear related to your health, your family, your job, and the economy. Although no one knows exactly what the next weeks or months will hold, many strategies can successfully address the anxieties that emerge during this time.
These include physical steps, such as prioritizing sleep and staying active, and emotional support such as challenging unhealthy thoughts and calling family and friends.
If you deal with overwhelming anxiety, you know it can affect your entire being. Your mind may be filled with fear and visions of future coronar tragedies evolving . Your body will tense as your fight, flight, or freeze system kicks in. And you may feel spiritually depleted as the internal battle saps your energy.
How can I manage my anxiety during the coronavirus outbreak?
While there are many specific types of anxiety, one of the most common is Generalized Anxiety Disorder (GAD), which affects more than 6 million Americans. While it is normal to worry, those diagnosed with GAD have difficulty controlling worry on more days than not for a period of over six months and have three or more common symptoms:
- having a persistent sense of impending doom or danger, being irritable and on-edge, rapid breathing, constant trembling, feeling weak or tired.
- having difficulty concentrating or trouble sleeping.
- having an increased heart rate.
As the pandemic continues to spread, anxiety does as well. Keeping calm is key to both mental health and immune function.
Establishing a daily routine, checking the news during designated times, practising meditation, and reaching out to loved ones are some of the tips that help keep anxiety in check.
For these people, the COVID-19 pandemic may create an elevated fear of catching or dying from the virus. Anxiety sufferers are prone to catastrophizing, which can result in behaviors like panic buying or trying different medications and treatments in an effort to “cure” or prevent coronavirus.
There is currently no known cure or proven medication for COVID-19 at the moment. They can also fall victim to compulsively checking the news, scrolling and scrolling for something more definitive that just won’t come.
On the positive side, those who have been in treatment for an anxiety disorder might actually be better prepared for the current situation as they already have some coping mechanisms in place to deal with their day-to-day fears. But, for some, this could also be a tipping point that makes them paralyzed by that fear.
What are effective strategies to cope with stress?
One coping strategy to try is what some psychiatrists call “being with your fear.” It involves identifying what is currently causing your fear in a particular moment, then acknowledging that you and your body are currently safe.
Practice deep breathing and ground yourself in that breathing. Mental health and mindfulness apps like Headspace can be great places to get guided meditation tips and techniques.
It’s also crucial to stay virtually connected, be that with your doctor, or friends and family. We are social creatures by nature, and it’s been shown that social support buffers stress and anxiety. Try designating at least one phone call a day to a completely non-coronavirus related conversation, focusing instead on positive questions and stories.
Recognize the symptoms of stress—such as difficulty concentrating, irritability or sadness, and sleep problems—to know when and how to respond. Control what you can, but then try to release the concerns that you cannot control. Additionally, limit news consumption and practice self-care.
Resources For Anxiety
If you find yourself feeling overwhelmed and unable to cope, there are plenty of resources available. Many doctors and mental health providers are setting up virtual practices to help their patients keep up with their treatment.
You can also check out the Substance Abuse and Mental Health Services Administration (SAMHSA) for videos, treatment options, and up-to-date information and programs that can help. In addition to talking to your doctor and loved ones, experts also recommend joining a virtual support group around things like knitting or baking or another hobby or topic you enjoy.
These can be a form of positive distraction, which is a key coping mechanism for those with anxiety.
How do I cope with losing my job?
Our jobs are often tied to our identity, and you are allowed to grieve this loss. As you move forward, recognize that you are more than your title, challenge internal narratives "I will never find another job” and establish a daily routine as you search for a new position.
The following article covers this subject in detail, both seasonal flu viruses (which include influenza A and influenza B viruses) and COVID-19 are contagious viruses that cause respiratory illness. follow the link to read more on this.
Depression and COVID-19
While we all have bouts of sadness from time to time, for the 17.7 million people diagnosed with clinical depression, that grief and sadness is constant and comes with other symptoms like exhaustion, trouble sleeping, a shrinking appetite and/or overeating, sudden crying spells, and sometimes thoughts of suicide.
Just as with anxiety, the fear and isolation can be very dangerous for those with depression, because without an outside influence to remind them of the good, they may instead focus solely on the bad news and develop a skewed sense of the situation, and potentially not be able to pull themselves out of that spiral.
Depression sufferers may have a growing sense of hopelessness or be paralyzed by their fear, leading them to neglect themselves and their health. Loneliness and fear can also be triggers for suicidal thoughts.
Coping Tips For Depression
Which is why the two most important steps for those with depression right now are to focus on connection and self-care. It’s critically important, our experts say, to reach out to your social connections to remind yourself you are not alone.
And, while it may seem silly when you’re stuck indoors and not seeing anyone, having a daily routine of self-care can help ensure you don’t fall victim to your worst impulses. Get up, take a shower, get dressed, work out, cook your meals, make daily virtual “dates” with the people you love—your mind may be telling you to stay in bed and not do anything, but this will only make things worse.
Another coping skill is what our experts call “fake it to make it.” Basically, read or watch or do something that is the opposite of how you are feeling.
Don’t turn on that ultra-sad movie because you are feeling down, put on something funny and lighthearted instead. Focus on positive topics and distract yourself from that fear and sadness and loneliness.
Resources For Depression
If you find yourself struggling, be sure to notify your psychiatrist or other mental healthcare provider and try and schedule sessions. National Suicide Prevention Lifeline is available 24 hours a day, seven days a week.
Talk to someone, anyone in your network if you are seriously struggling—social connection can help alleviate some of that loneliness or fear that may be causing you to think irrationally or to follow unsafe impulses.
Some local lawmakers are also calling for mental health professionals to offer free mental health sessions over the phone or online to help anyone who might be struggling right now. Go to the National Alliance On Mental Illness to search for free support and education programs in your area.
OCD and Coronavirus
Obsessive compulsive disorder is a type of anxiety disorder that happens when a person gets stuck in a cycle of obsessions and compulsions. Obsessions are considered any thoughts, images, or impulses that recur frequently and feel outside of your control to stop or manage.
Compulsions are repetitive physical behaviors or thoughts that someone might use in an attempt to make their obsession go away. Most people with OCD are able to recognize that their compulsions will not make obsessions go away, but fall victim to them as they appear to be the only way they can cope or escape.
For those with OCD, specifically those whose obsessions and compulsions that revolve around cleanliness and germs, a global pandemic is their worst nightmare come to life. The CDC recommends hand washing and home sanitizing “frequently,” but that can be taken to the extreme by those with OCD.
Instead of washing their hands for 20 seconds every time they’ve been outside or coughed and sneezed, they may find themselves scrubbing their hands raw under scalding hot water for 20 minutes in an effort to feel “clean.” Stress around the virus can also trigger compulsions around counting or checking things, according to our panel.
Coping Tips For OCD
Just like those with anxiety, people with OCD need to carefully read the instructions and advisories from the CDC and WHO to learn what the appropriate precautions are that they should be taking and to what extent.
For someone with OCD, part of the treatment could be trying to cut back on behaviors like excessive washing, so during this particular crisis give yourself permission to follow the guidelines, washing hands frequently and/or using hand sanitizer, opening take out containers outside, disinfecting surfaces like light switches and remotes.
Another aspect that’s unique to someone with OCD is the idea of trust. People with OCD may not trust their own assessment of what’s going on around them. They second guess their own reactions. Here, it’s important to know, yes this is a big deal; and yes, it is uncertain and extreme.
To much news can make anyone start to spiral, but it’s especially important for someone with OCD to limit their time. Literally, five minutes a day is all that’s recommended. It’s not a lot but going beyond that could get you hooked.
On the plus side, someone with OCD has above average skills for managing anxiety. They may actually be more adept at dealing with all the upheaval the rest of us are struggling with.
Resources For OCD
If you are someone who has been seeking treatment for your OCD, make sure you are using those coping mechanisms you have learned in earnest and reach out to your doctor or mental health professional if you find your compulsions are becoming exacerbated by the stress.
The International OCD Foundation is a great resource if you need help finding a doctor or if you are looking for a support group to help get you through this challenging time. Being able to speak with others also dealing with your same struggles can be helpful in coping and lessening your episodes.
Substance Abuse Disorder and COVID-19
An all-too-common disorder that affects a wide spectrum of age, race, and socio-economic groups, substance abuse disorder is a disease that affects the brain and behavioral patterns, causing a person to be unable to control their use of addictive substances like alcohol, tobacco, illegal drugs, and prescription medication.
Many people with a substance abuse problem also suffer from another form of mental illness—over 9 million adults, according to the most recent data from NAMI.
The big concern for those in treatment for substance abuse is the risk of relapse. Many of those in treatment for substance abuse rely on daily meetings or support groups like Alcoholics Anonymous.
As our experts note, while addiction is treatable, no one can recover alone. With isolation and lockdowns in place, many people aren’t able to get the support they need to help battle their urges.
Coping Tips For Substance Abuse Disorder
For those that are struggling, find someone immediately to be a recovery mentor. This could be a sponsor, a recovery coach, or a therapist.
Connect with them as much as you can or as much as you think you need to, but be sure you are talking about what substance abuse experts call the four major points of connection each time:
Everything that’s going on, everything that you are feeling, everything that you are thinking, and everything that you are doing in that moment.
If you find yourself having increased cravings, you need to talk to someone—a friend, a loved one, anyone you feel comfortable opening up to — even if that means calling a new person every 10 minutes. Whatever you can safely do to avoid the isolation that could lead to a relapse.
Additionally, substance abuse experts recommend giving yourself daily “talks” to remind yourself what succumbing to your cravings will result in. Talk to yourself about everything good that will happen if you don’t addict and everything bad that will happen if you do. Ask what is triggering the craving and what you can do to help soothe and distract yourself.
Things like regular exercise, reading a good book, playing a video game, and picking up a new hobby can all be helpful distractions.
Resources For Substance Abuse Disorder
Groups like In The Rooms, Self-Management and Recovery Training, and Alcoholics Anonymous all provide helpful programs and online support groups to assist those with substance abuse issues and help them navigate their addiction remotely.
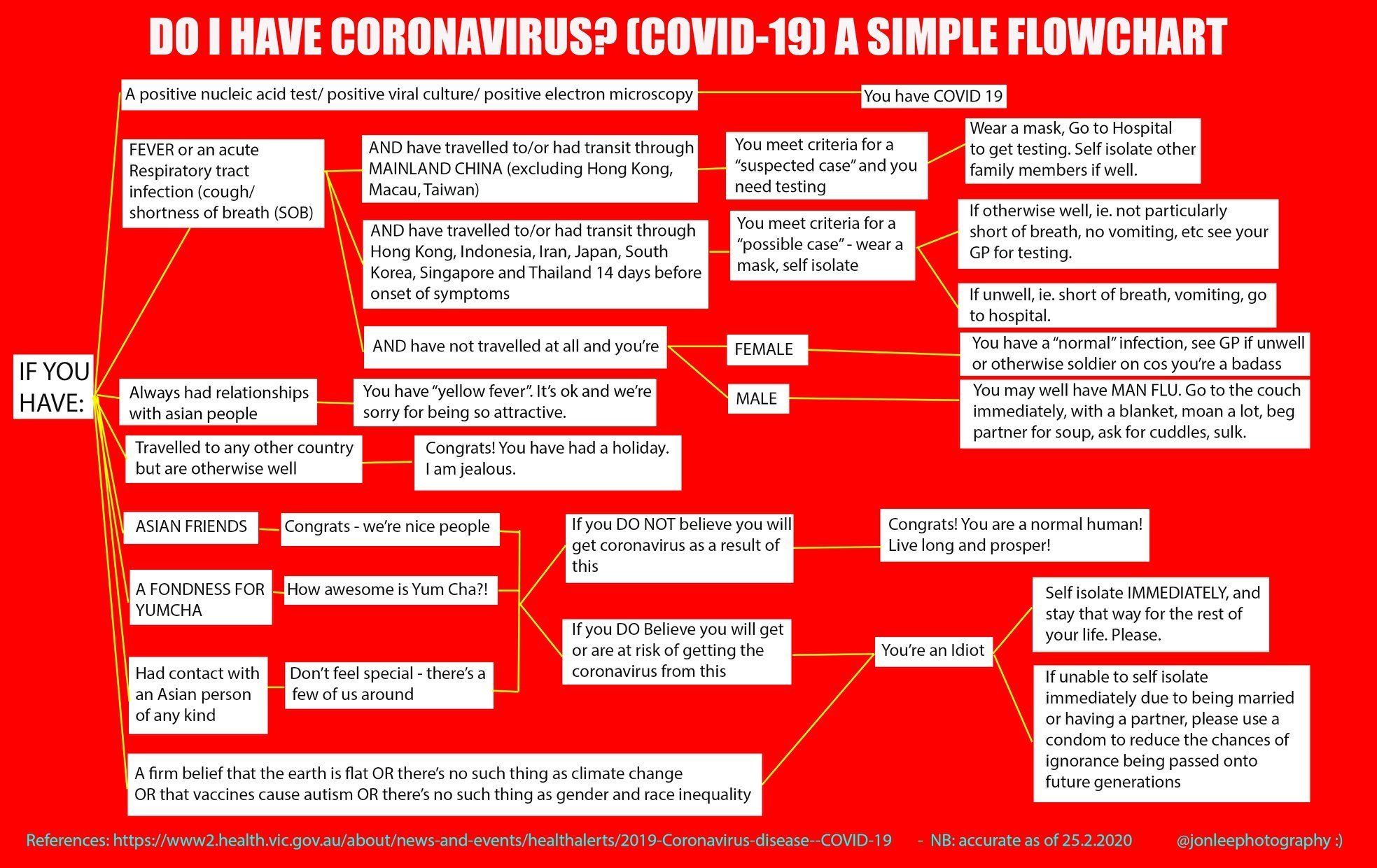
The following was sent from an Asian friend and takes a light hearted look at coronavirus.
Parenting and Family Help
COVID-19 and the social distancing measures that followed have completely upended daily routines and family dynamics. Specific strategies can help you navigate the new normal, from soothing your children to keeping your pet safe.
How can I help my child process the pandemic?
Children may feel confused, angry, or restless during the outbreak. Here is how to navigate their feelings and yours when everyone is under one roof: Validate complicated feelings, process emotions through play, and embrace structure and routine.
How do I homeschool my child?
One strategy is to lean on your community. Assemble a group of parents who can each contribute one remote lesson, such as an English class or cooking demonstration. In addition to keeping kids engaged and social, this joint effort affords off-duty parents time to work, run errands, and keep up with household responsibilities.
How can I maintain a healthy relationship with my partner when we are both home all day?
Social distancing has erased the typical relationship cycle of periods apart and periods together. Being in the same place may require you to take space by working in different parts of the home. Recognize that both people may not cope in the same way, and step away when you are upset, along with other measures.
How can my family function under one roof?
Carve out specific times and places for everyone to do their work. After everyone is finished for the day, try to appreciate the old-fashioned family time everyone can spend together, such as watching one TV show or movie.
Will my pet contract COVID-19?
There have been no reports of pets contracting COVID-19, but until more information is available, people with the illness should avoid close contact with their pets, such as cuddling or kissing them. People can also establish emergency plans regarding their pets care, food, and medication in the event of hospitalization.
Staying Connected
Humans are innately social, and it’s difficult to refrain from seeing family, friends, and the people we simply pass on the street every day. Many are calling for social distancing to be reframed as “physical distancing,” to emphasize the importance of staying connected during this time.
How can I feel less lonely while social distancing?
Video-chatting with friends and family is critical, and aim to schedule regular calls rather than single calls. Shift activities like book clubs and happy hours online. Immerse yourself in a fictional world, as characters can serve as “social surrogates.” Acts of kindness toward others can also alleviate loneliness by instilling a sense of connection and purpose.
How do I maintain my relationships while self-quarantining?
Humans have a pervasive, evolutionary drive to be with other people—which can make social distancing incredibly tricky. Maintain your relationships by calling and video-chatting people you see regularly, and take advantage of the opportunity to deepen relationships with people who you are not as close with yet.
Eating Disorders and Coronavirus
There are three main types of eating disorders: anorexia nervosa, bulimia nervosa, and binge-eating disorder. People with anorexia tend to be obsessed with their weight, drastically restricting their calorie intake and extreme amounts of exercising, constantly thinking they are overweight even when they are in fact dangerously underweight.
For those with bulimia, their disorder is typified by periods of uncontrollable binge eating, followed by a sensation of being painfully full and the need to “purge” in an attempt to compensate or get rid of the calories they now feel guilty for consuming.
Binge-eaters will also experience that same urge to eat and inability to control how much they eat, but they do not practice purging or calorie restrictions post-binge.
For those with eating disorders, the main concern is around the perceived fear of lack of supplies. Those with an eating disorder may believe they need to hoard food; due to the consistently empty shelves they see at the grocery store. They may also find a reason to use these non-existent food shortages as an excuse to deprive themselves of food as a form of rationing.
Coping Tips For Eating Disorders
It’s important for those with eating disorders to recognize that despite the empty shelves they may be seeing, the USDA and food manufacturers have assured Americans that there are not currently any food shortages or disruptions in the food supply chain.
The empty shelves are a result of panic-buying and employees unable to stock shelves fast enough to keep up with demand. While ensuring you have enough food to last you if you do face a self-quarantine is a smart option, that only equates to about two weeks of food.
Try and focus on buying fresh veggies and fruits, whole grains, lean protein, and foods rich in calcium and vitamin C. Taking vitamin D to compensate for lack of exposure to sunshine is also highly recommended.
And, while exercising daily is a healthy choice, don’t take it to the extreme. Aim for 20-30 minutes of moderate exercise, not three hours of intense cardio.
Resources For Eating Disorders
If you feel nervous or that you might be slipping into dangerous patterns, reach out to a nutritional counselor or your doctor to talk through your concerns.
You can also find online support from the National Eating Disorders Association, Eating Disorder Foundation, and National Association of Anorexia Nervosa and Associated Disorders.
Like substance abuse, eating disorders are a form of addiction, meaning it’s important to maintain social contact daily with someone to help support your recovery and management of your addiction.
ADHD and COVID-19
Attention-deficit/hyperactivity disorder (commonly known as ADHD) is a behavioral disorder that causes someone to suffer from inattention and difficulty focusing, along with hyperactivity, fidgeting, and impulse control issues.
While most people relate ADHD to children, many adults also suffer from ADHD, which can lead to major disruptions in their daily life. This can include everything from work performance to relationships.
One of the main problems for those with ADHD who are stuck at home during the COVID-19 outbreak is a severe decline in productivity. With most people working from home and many companies having to lay off percentages of their workforce, now is not the time to look as if you are slacking on the job.
Another concern our experts have is that, due to their inability to focus or stay on task, some patients with ADHD may not be able to follow the strict guidelines for protecting you and your loved ones against the spread of infection. ADHD patients may forget to wash their hands frequently or find it hard to stay inside.
Coping Tips For ADHD
If you have ADHD, doctors can’t stress enough the importance of setting a daily schedule and sticking to it. Getting up at the same time each day and following a set pattern can help you maintain your concentration and keep being productive and responsive at your job.
It’s ok to take breaks, as long as you structure them to include set activities for a limited amount of time — no scrolling on Instagram for two hours when you should be writing up that TPS report.
Be sure to practice self-care, including daily exercise. If you need guidance, many gyms have switched to online streaming of their classes, or you can check out fitness apps like WellBeats or Down Dog.
If your child has ADHD and usually has the support of some kind of accommodations in school, you can try to replicate that at home by breaking up assignments into short sessions, avoiding redundant tasks, and keeping instructions simple and straightforward. A few apps that are worth checking out: Dreambox (for math), Flocabulary (for vocab), and iReward Charts (to track progress).
Resources for ADHD
If you feel like you aren’t able to successfully manage your ADHD during this crisis, reach out to your mental health professional for guidance, or check in with organizations like Children and Adults with Attention Deficit/Hyperactivity Disorder (CHADD) and Attention Deficit Disorder Association (ADDA) for virtual peer support groups and helpful tips.
Bipolar Disorder and Coronavirus
Bipolar disorder, (formerly known as manic depressive illness or manic depression), is a mental health disorder where people experience two distinct types of extreme emotional shifts identified as manic episodes and depressive episodes. When someone is having a manic episode, they experience what are considered “up” periods of emotions that include irritability, excitability, elation, and being energized. These are sometimes followed by “down” periods characterized by sadness, indifference, and hopelessness.
Like anxiety and depression, the stress and fear caused by COVID-19 can trigger these abnormal behaviors, specifically manic episodes, which can then be followed (although not always) but very intense depressive episodes.
Coping Tips For Bipolar
According to our pro panel, one of the most helpful things you can do for yourself right now, in addition to self-care and daily connections with friends and family, is to self-monitor your habits by keeping a diary or journal. Pay particular attention to your sleep, as a disruption in those nightly patterns is a key indicator that you might be experiencing more episodes.
It’s also important to ask loved ones to check in on you (virtually), as they are more likely to be able to identify behavioral and mood shifts. If that’s the case, consult with your psychiatrist or whichever doctor manages your prescription to consider altering your medication levels.
Resources for Bipolar
For support, look to SAMHSA and NIMH for 24/7 helplines, as well as support groups like the Depression and Bipolar Support Alliance.
Schizophrenia and COVID-19
Hallucinations, delusions, and impaired behavior are all symptoms of schizophrenia, a mental health disease that results in people being unable to interpret reality normally. They can act and speak erratically and may have trouble communicating or controlling some movements. They are also prone to suicidal thoughts.
For many of us, this strange new world we’re living in due to COVID-19 can feel like some sort of alternate reality. For those suffering from schizophrenia, it creates a very dangerous situation, as their perception of reality can already be warped.
People who have schizophrenia and are able to successfully function in their community most likely are able to do so through medication, a regular routine, and an array of support that could include physicians, caseworkers, and peer groups.
With COVID-19, all of this has been disrupted and they are now in a place of isolation that could make them a danger to themselves. If you are someone already prone to see the world through a paranoid lens, you may believe the misinformation about coronavirus that is circulating, or even be seeking it out to help make the news fit your version of reality.
Coping Tips For Schizophrenia
Our experts stress that maintaining daily check-ins with your doctor and, if possible, caseworker, is absolutely a necessity in making sure you don’t become fixated on delusions or hallucinations that may emerge due to increased stress.
Again, having a set daily routine is important in ensuring you are keeping some semblance of normalcy in your life during this upside-down time.
And maintaining your regular medication is crucial, so be sure to stay on top of your prescription refills and don’t wait to the last minute to get them filled.
Resources for Schizophrenia
If you are having suicidal thoughts, call the National Suicide Prevention Lifeline and contact your mental health provider immediately.
Post Traumatic Stress and Coronavirus
For anyone who has been exposed to a type of trauma, post-traumatic stress (PTS) is a common condition that can occur. It is most typically associated with military veterans, but is also something that can happen after traumatic events that range from car crashes and natural disasters to sexual abuse survivors.
Symptoms of PTS include reliving the event (a.k.a. flashbacks), nightmares, avoiding certain places or activities that remind you of the trauma, paranoia, isolation, and hyperawareness.
Coping Tips For PTS
According to our experts, people with PTS will most likely not be too severely impacted by coronavirus, as the majority of their symptoms are triggered by things that remind them of the traumatic event.
That said, stress can cause you to become emotional and fearful, especially if you are still processing the event.
One thing to do is reframe the idea of what a good day means for you. In these uncertain circumstances, some degree of stress and anxiety is normal and expected. Feeling a sense of control over things may help. Think about what you can do and set simple goals.
Thoughts of contracting the virus may cause you to feel stressed and may make you associate the virus with the traumatic event that caused your PTS. You may find you have a harder time sleeping and concentrating is more difficult because of this association.
Resources for PTS
The National Center for PTSD is a great resource if you are looking for help connecting with a professional who specializes in PTS.
It also provides some helpful self-coping strategies to use if you are feeling overwhelmed and are unable to speak with someone immediately when symptoms appear.
Know that for many with this condition, you can’t always escape the things that trigger you, however being able to identify those triggers can help you better manage and learn how to face your fear.
Physical Health

Following the guidelines put forth by the World Health Organization and the Centers for Disease Control and Prevention is critical so that everyone stays safe. From handwashing and social distancing to boosting the immune system, individuals can take plenty of concrete steps to maintain their health.
What will convince people to stop the spread?
Efforts to raise the alarm and push people to change their behaviour following health guidelines are potentially useful if done carefully and with clear solutions provided. Some people—such as peers or familiar experts—may be more persuasive in these efforts than others.
How do I break the habit of touching my face?
Identify when and why you unconsciously touch your faces, such as during periods of boredom or stress. Address those triggers by keeping something in your hand to fidget with, such as a beaded bracelet, or by putting your hands between your legs to make touching your face more difficult.
How can I boost my immune system?
Keep your immune system healthy by getting plenty of sleep, exercise, and eating nutrient-rich foods like leafy greens and fruit. Stress hormones can tax the immune system, so soothing your stress can help as well.
Are there long-term psychological effects for those who have contracted the virus?
Data from other outbreaks, including SARS (also a coronavirus) indicates that in the medical profession where one study was conducted, some people perceived that colleagues shunned them.
Remote Work

To maximize social distancing, more and more companies are asking employees to work from home. In many locations, it is now required by law that nonessential workers stay home, meaning that those who can work remotely must do so.
Even in the best of times, transitioning to working from home can be a significant adjustment. During a pandemic, added anxiety and new distractions—such as children attending school from home, too—have made the shift more challenging than ever.
Adopting strategies to minimize distractions, as well as accepting that perfect productivity may be out of reach during this stressful time, can help individuals adapt to their new work life.
How do I learn to work virtually?
Establish a clear structure to your workday and draw distinct boundaries between work and other areas of your life. This means setting up a dedicated workspace (if space allows), starting and stopping at set times, and “getting ready” each day—showering, getting dressed, and having breakfast—before beginning work.
How can I improve my productivity during this time?
Transitioning to remote work provides the opportunity to test out new workstyles and strategies. Experiment with different time management and collaboration strategies—such as planning out a weekly schedule or setting up a daily check-in with coworkers—to identify ways to become more productive.
How can I best manage my employees remotely?
Many workers are under tremendous personal or economic stress. Managers can help by being transparent about any challenges the company will face, allowing for greater flexibility and autonomy, and providing opportunities for social connection (such as video meetings) to help reduce feelings of loneliness or anxiety.
How can I work when I am anxious?
Focusing on work while your mind is buzzing with anxiety can be immensely challenging. Remind yourself that feeling anxious right now is normal. Limiting news exposure, practising healthy habits, and being kind to yourself can soothe anxiety and help reset your focus.
Remote Therapy: Moving to Phone and Video Sessions

Therapy sessions are typically conducted face to face, but the COVID-19 outbreak is pushing therapists and clients to adapt. To keep therapy going strong, many are turning to video-chat apps or phone calls. Even remote conversations can produce effective treatment, but if this is the first time planning an online session, there are some details worth considering.
How do I make the most of remote therapy?
There are steps you can take to prepare for your sessions. These include testing out the app or software you will be using, making sure you have enough privacy during your session, and limiting distractions by closing other apps or websites. You will want to know your therapist contact information and preferred means of payment, too.
My therapist will not continue therapy remotely. What should I do?
Your therapist may refer you to someone who can provide therapy remotely for as long as is needed. If not, many other therapists offer remote sessions. If you do not want to see a new therapist, you can ask your therapist about books, online resources, and activities that can help until your next session.
Is remote therapy as effective as in-person therapy?
Certain therapies seem to be just as effective when delivered over the phone. One study found that cognitive behavioural therapy was equally successful in treating depression when administered by telephone or face-to-face, and fewer people discontinued treatment over time.


[…] you have any history of anxiety, trauma, or panic attacks, the coronavirus may have pushed your fear to intolerable […]