Tardive Dyskinesia: The Invisible Danger Lurking in Your Medications
Lesson 2
Welcome to the intricate world of Tardive Dyskinesia (TD), a condition often shrouded in complexity and misunderstanding. As we embark on this journey, we’ll unravel the layers that define Tardive Dyskinesia, its impact on lives, and the latest strides in treatment.
The following sections delve into the causes, symptoms, and personal stories that bring the reality of living with Tardive Dyskinesia to light. Get ready to explore the nuances of this movement disorder, its prevalence, and the evolving landscape of care and support for those affected.
Table of Contents
Key Takeaways
Defining Tardive Dyskinesia (TD)
The Impact of TD on Patients’ Lives
The Causes of Tardive Dyskinesia
The Role of Antipsychotic Medications in TD
How Dopamine Receptor Blockage Leads to TD
Identifying the Symptoms of Tardive Dyskinesia
Common Physical Manifestations of TD
The Range of TD Severity and Patient Experiences
Prevalence and Risk Factors
Statistical Overview of TD Occurrence
Populations at Higher Risk for Developing TD
Treatment Options for Tardive Dyskinesia
The Effectiveness of Newer Antipsychotics in Reducing TD Risk
The Evolution of Tardive Dyskinesia Understanding
Historical Perspective on TD Recognition and Diagnosis
Advances in Treatment and Management
Living with Tardive Dyskinesia and its Comorbidity on mental health and movement disorders
The Daily Reality for Individuals with TD
Coping Strategies and Support Systems for treatment, recovery, and maintaining health and wellness
The Role of the FDA and Medical Community
Regulatory Approvals for TD Treatments
The Importance of Patient Awareness and Doctor-Patient Communication
Tardive dystonia vs. tardive dyskinesia
Parkinsonian with Tardive dystonia and Dyskinesia
Key Takeaways
Defining Tardive Dyskinesia (TD)
Tardive Dyskinesia (TD) is a neurological syndrome characterised by involuntary and repetitive movements of the face and body. It stems from prolonged use of certain medications, particularly antipsychotics that are prescribed for mental health conditions like schizophrenia and bipolar disorder.
These movements can range from rapid blinking to grimacing, lip-smacking, and even tongue protrusion, often leading to considerable discomfort and social stigma for patients. TD may also include involuntary movements of the limbs, fingers, or torso, which can be swift, jerky, or dance-like.
While the condition primarily affects the orofacial muscles, it can spread to other parts of the body, causing distressing and sometimes disabling symptoms.
The curious aspect of TD is its persistence; symptoms can endure long after the causative medication has been discontinued. This permanence marks a stark contrast to other drug-induced movement disorders, which typically resolve after the drug is stopped.
For more in-depth information, Tardive Dyskinesia can be understood as a chronic condition that may require ongoing management and treatment.
The Impact of TD on Patients’ Lives
Tardive Dyskinesia (TD) reaches far beyond its physical manifestations, profoundly affecting the lives of patients. The involuntary movements characteristic of TD can lead to emotional and psychological distress as individuals struggle with the unpredictability and visibility of their symptoms.
This struggle often extends into social spheres, where the fear of judgment or misunderstanding from others can result in isolation and withdrawal. The stigma associated with TD not only impacts personal relationships, but can also create barriers to employment and public engagement, further diminishing quality of life.
Patients may grapple with the duality of their condition—managing the mental health disorder for which the antipsychotics were prescribed while simultaneously coping with the side effects of the same medications.
This double burden can complicate treatment decisions and may lead to an avoidance of necessary medicines for fear of exacerbating Tardive Dyskinesia symptoms.
Moreover, the chronic nature of TD means that patients must adapt to a potentially lifelong condition. The need for ongoing treatment, the uncertainty of symptom progression, and the absence of a cure add layers of complexity to an already challenging existence.
The Causes of Tardive Dyskinesia
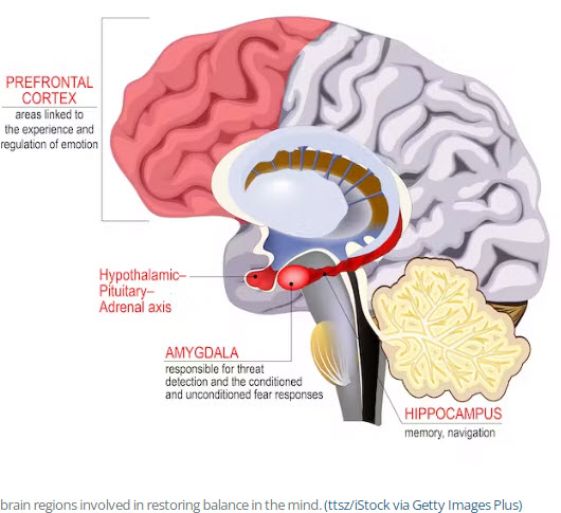
The roots of Tardive Dyskinesia (TD) are primarily entrenched with the prolonged use of antipsychotic medications. These medications, designed to treat conditions like schizophrenia, bipolar disorder, and severe depression, often block dopamine receptors in the brain. The blockade of these receptors is pivotal in managing symptoms of psychosis, but it also disrupts the neurological pathways that control movement.
Over time, this disruption may lead to the development of TD, with the risk increasing the longer these medications are taken. According to WebMD, the risk is not uniform across all antipsychotics; older, “typical” antipsychotics carry a higher risk compared to their newer “atypical” counterparts. Moreover, the onset of TD symptoms can vary from a few months to several years after initiating treatment with antipsychotics, adding to the unpredictability of the condition.
It is also understood that not everyone on antipsychotic medication will develop TD, indicating that individual biological factors play a role. These factors could include genetic predispositions, age, and the presence of other health conditions. Understanding these nuances is essential for both patients and healthcare providers to make informed decisions regarding the management of psychiatric disorders and the mitigation of potential side effects.
The Role of Antipsychotic Medications in TD
Antipsychotic medications play a pivotal role in the development of Tardive Dyskinesia (TD), a condition marked by involuntary muscle movements. These drugs, essential in treating severe mental health disorders, exert their therapeutic effect by altering brain chemistry, specifically targeting the neurotransmitter dopamine.
Dopamine pathways in the brain are crucial for regulating movement, and antipsychotics work by blocking dopamine receptors. This blockade can effectively reduce symptoms of psychosis, but it also creates a significant side effect: the risk of TD. Over time, this disruption in dopamine signalling can lead to the development of the erratic and uncontrollable movements characteristic of TD.
The risk of TD increases with the duration of antipsychotic medication use, and it is more commonly associated with older, first-generation antipsychotics. However, even newer, second-generation antipsychotics, which were initially thought to pose a lesser risk, have been implicated in Tardive Dyskinesia cases.
The complexity of TD’s relationship with antipsychotic medications underscores the need for careful monitoring and management of patients undergoing treatment.
To understand this balance between benefit and risk, WebMD provides a comprehensive look at how these medications impact individuals and the mechanisms behind their side effects. Patients and healthcare providers must work together to navigate the challenges posed by antipsychotic drugs and their potential to cause Tardive Dyskinesia.
How Dopamine Receptor Blockage Leads to TD
Identifying the Symptoms of Tardive Dyskinesia
Dopamine, a critical neurotransmitter in the brain, regulates motor function and reward pathways. Antipsychotic medications, which are used to treat mental health disorders, target the dopamine system to alleviate symptoms of psychosis.
By blocking dopamine receptors, particularly the D2 subtype, these medications can mitigate hallucinations and delusions. However, this same action can disrupt normal motor function, leading to Tardive Dyskinesia (TD).
The blockage of dopamine receptors is akin to creating a dam in a river; it causes a build-up of neurotransmitter activity elsewhere. When the flow of dopamine communication is interrupted, the brain attempts to compensate by making the receptors more sensitive or by increasing the number of receptors.
This overcompensation can result in the brain signalling for movements that are not needed, manifesting as the uncontrollable movements seen in tardive dyskinesia. For those wanting to dive deeper into the effects of dopamine receptor blockage, the National Institute of Neurological Disorders and Stroke provides a wealth of information.
This heightened sensitivity and receptor proliferation can persist even after the medication is stopped, which is why TD symptoms can continue indefinitely, creating a long-term challenge for patients.
Identifying the Symptoms of Tardive Dyskinesia
When pinpointing Tardive Dyskinesia (TD) symptoms, healthcare professionals look for distinctive involuntary movements that primarily affect the facial and oral regions. Patients may exhibit rapid blinking, grimacing, or involuntary movements such as lip-smacking, puckering, and chewing.
These symptoms can extend to the tongue, causing protrusion or curling and interfering with speech and eating. TD also affects the limbs, with patients experiencing jerky or twisting motions in their arms and legs and twisting movements of the fingers. These physical symptoms can be subtle initially, often starting slowly and then increasing in intensity over time.
In some cases, TD can present with respiratory irregularities, such as grunting and difficulty breathing due to affected muscles. These symptoms are not uncommon to fluctuate, with periods of less noticeable movements followed by more pronounced episodes.
For those seeking a deeper understanding of the nuances of TD’s physical manifestations, the Cleveland Clinic offers an in-depth exploration. Recognising these signs is vital for prompt diagnosis and management, as early intervention may help mitigate the severity and progression of Tardive Dyskinesia.
Common Physical Manifestations of TD
Tardive Dyskinesia (TD) often reveals itself through a spectrum of involuntary muscle movements that are both distinct and distressing. These movements primarily target the orofacial area, where patients might experience rapid, uncontrollable blinking or persistent grimacing that they cannot suppress.
The mouth is particularly susceptible, with symptoms such as lip-smacking, puckering, and chewing motions occurring without the patient’s intent. These involuntary actions can extend to the tongue, leading to uncomfortable protrusion, twisting, or curling that can interfere with everyday speech and eating.
In some individuals, TD manifests through movements beyond the face, affecting the upper and lower limbs. Patients may notice their fingers performing piano-playing or fly-catching motions, and their arms and legs may execute jerky or twisting actions.
Such movements can be erratic and complex and fluctuate in intensity, often becoming more pronounced with stress and subsiding during focused activities or sleep. For a more detailed look into these symptoms, the Cleveland Clinic provides a comprehensive overview.
Recognising these signs early is crucial, as they are the hallmarks of tardive dyskinesia and the indicators for healthcare providers to evaluate the need for potential treatment changes.
The Range of Tardive Dyskinesia Severity and Patient Experiences
Tardive Dyskinesia (TD) is a broad spectrum of severity, ranging from mild twitching to severe, disabling movements. Patients with mild TD might experience subtle tics or tremors, often overlooked or dismissed as nervous habits.
These minor symptoms can be annoying, but they typically don’t interfere significantly with daily activities. Conversely, severe cases of TD can be life-altering, with pronounced and relentless movements that challenge the simplest tasks.
Patients may struggle with activities that require fine motor skills, such as writing or buttoning a shirt, and face difficulties with speaking and eating due to uncontrollable facial muscle contractions. The variability in experiences and the impact on quality of life is profound, as some individuals navigate the condition with minimal disruption. In contrast, others endure a stark transformation of their day-to-day existence.
The unpredictable nature of TD symptoms also contributes to emotional distress as patients cope with the uncertainty of their condition’s trajectory. It’s not just the physical toll that weighs heavily; the psychological burden of living with a visible and misunderstood disorder can be equally challenging, shaping the patient’s experience in a profoundly personal way.
Prevalence and Risk Factors
Tardive Dyskinesia (TD) is not a rare occurrence among those taking antipsychotic medications, with prevalence rates hovering around 20-30% for those on typical and atypical antipsychotics, respectively. This variation underscores the importance of monitoring and selecting appropriate treatment courses. The risk factors for developing TD encompass a range of demographic and treatment-related elements, including age, gender, and the duration of medication use.
Elderly patients, particularly women, exhibit a higher propensity for tardive dyskinesia, suggesting a possible link with hormonal or metabolic changes. Moreover, individuals with mood disorders, such as depression or bipolar disorder, who are treated with antipsychotics also face an elevated risk. The intricate interplay of these factors calls for a personalised approach to medication management, with vigilant assessment for early signs of TD.
The longer the duration of antipsychotic treatment, the greater the likelihood of developing TD, highlighting the critical balance between therapeutic benefits and potential long-term side effects.
Genetic predispositions, alongside other health conditions, further complicate the risk landscape, demanding that healthcare providers remain astute to each patient’s unique profile. Understanding these nuances is vital for mitigating the impact of TD and ensuring that patients receive care that is both effective and considerate of their overall well-being.
Statistical Overview of TD Occurrence
Tardive Dyskinesia (TD) emerges as a notable concern among patients undergoing antipsychotic therapy, with prevalence rates that command attention. According to statistical data, approximately 20% of patients treated with atypical antipsychotics and a higher rate of around 30% for those on typical antipsychotics experience tardive dyskinesia
These figures highlight the significant impact of medication type on the likelihood of developing this condition. Several factors, including the duration of antipsychotic use and patient demographics, influence the variability in tardive dyskinesia occurrence.
Long-term treatment with antipsychotics is strongly correlated with an increased risk of TD, emphasising the need for cautious medication management. Moreover, specific populations, such as older people and women, are more susceptible to TD, suggesting a potential intersection with biological differences.
Understanding these statistical nuances is crucial for healthcare providers to tailor treatment plans that minimise the risk of TD while effectively managing psychiatric symptoms.
Populations at Higher Risk for Developing TD
Certain groups of individuals stand at a heightened risk for developing Tardive Dyskinesia (TD), a condition characterised by involuntary, often persistent movements primarily affecting the face and body. Age is a significant factor, with older adults experiencing a more pronounced susceptibility to TD, particularly those who are prescribed antipsychotic medications as part of their treatment regimen.
This increased risk in the elderly may be attributed to age-related changes in brain chemistry and drug metabolism. Women, interestingly, also face a greater likelihood of developing TD, a disparity that could be linked to hormonal influences or differences in how medications are processed in the female body. Furthermore, individuals with a history of mood disorders, such as depression or bipolar disorder, and those receiving high doses of antipsychotic medication over extended periods are more vulnerable.
The intersection of these demographic factors—age, gender, and mental health history—creates a complex risk profile that necessitates vigilant monitoring by healthcare providers. For patients and caregivers seeking to understand this risk landscape, resources like the Cleveland Clinic offer valuable insights, emphasising the need for personalised medication strategies to minimise the potential for Tardive Dyskinesia.
Treatment Options for Tardive Dyskinesia

Navigating the treatment landscape for Tardive Dyskinesia (TD) requires a nuanced understanding of the condition’s complexities.
The FDA has given the green light to two significant medications: (1) valbenazine (Ingrezza) and (2) deutetrabenazine (Austedo), both of which have shown promise in reducing the involuntary movements characteristic of TD. These treatments work by modulating the levels of dopamine in the brain, targeting the neurotransmitter pathways that contribute to these uncontrollable muscle movements.
Apart from medication, patients may benefit from non-pharmacological strategies. Physical therapy, for instance, can enhance motor skills and muscle control, offering a complementary approach to managing symptoms. For those seeking a deeper dive into the pharmacological and non-pharmacological treatments available for TD, the National Institute of Neurological Disorders and Stroke provides a comprehensive resource.
It’s critical to tailor treatment to the individual, taking into account the severity of TD symptoms and the patient’s overall health profile. Regular consultation with healthcare providers ensures that treatment efficacy is monitored and adjusted as needed. This personalised care plan is pivotal in not only managing TD, but also in improving the patient’s quality of life.
The Effectiveness of Newer Antipsychotics in Reducing Tardive Dyskinesia (TD) Risk
The advent of newer antipsychotics has brought a glimmer of hope in the fight against Tardive Dyskinesia (TD). These modern medications, known as second-generation or atypical antipsychotics, have been engineered with a more nuanced approach to dopamine receptor blockage, seeking to minimise the risk of TD.
Compared to their predecessors, these atypical antipsychotics exhibit a lower affinity for dopamine D2 receptors, which is believed to correlate with a reduced incidence of TD. Studies have shown that patients on these newer medications experience TD at a rate of about 20%, a notable decrease from the 30% associated with older, typical antipsychotics.
This statistical difference, outlined in comparative studies, suggests a meaningful advancement in the safety profile of antipsychotic treatments. However, it’s imperative to recognise that while the risk is lessened, it is not entirely eliminated. Vigilant monitoring for early signs of TD remains a critical component of patient care, regardless of the generation of antipsychotic medication being used.
The nuanced pharmacology of these newer agents offers a balance between efficacy in treating psychiatric disorders and a more favourable side effect profile.
Their role in the therapeutic arsenal underscores the importance of individualised treatment plans that carefully consider the long-term implications of antipsychotic use.
The Evolution of Tardive Dyskinesia Understanding
The journey to understanding Tardive Dyskinesia (TD) has been a winding road, marked by evolving perceptions and deepening knowledge. Initially identified in the 1950s, it wasn’t until 1964 that the term “tardive dyskinesia” was coined, reflecting the condition’s delayed onset after long-term antipsychotic use.
This recognition was a crucial step in distinguishing TD from other drug-induced movement disorders, which were often temporary and resolved after medication cessation. As the years progressed, the medical community began to observe the nuances of TD more closely, recognising its potential persistence and the varying degrees of severity among patients.
It became apparent that the condition could continue indefinitely, posing a significant challenge for those affected. In response to these observations, research intensified, aiming to unravel the biological underpinnings of TD.
This quest for knowledge revealed the condition’s complex relationship with dopamine receptors in the brain, specifically how antipsychotic-induced blockage could lead to the characteristic involuntary movements. With the approval of treatments by the FDA, such as valbenazine and deutetrabenazine, the medical community made strides in offering relief to patients, marking a new era in the management of TD.
Today, the understanding of TD encompasses not just the physical symptoms but also the profound impact on patients’ mental health and quality of life, shaping a more compassionate and comprehensive approach to care.
Historical Perspective on TD Recognition and Diagnosis
The term “tardive dyskinesia” crystallised in the medical lexicon in 1964, a beacon illuminating a path for greater understanding of the condition. Before this formal recognition, the symptoms of TD often lurked in the shadows, unclassified and mingled with other movement disorders.
It is this pivotal moment in history that underscored the delayed onset of involuntary movements associated with prolonged use of antipsychotic medications. With a name came a more explicit focus; clinicians began to distinguish TD from other drug-induced motor disturbances, many of which were transient and resolved once the causative medication ceased.
This differentiation was crucial, as it acknowledged the unique persistence of TD symptoms and their potential to endure long after the discontinuation of antipsychotic therapy. In the ensuing years, they witnessed a burgeoning awareness within the medical community as the distinct features and challenges of TD came into sharper relief.
A concerted effort emerged to demystify the underlying mechanisms, leading to discoveries about the role of dopamine receptor blockage and the ensuing sensitisation. For a more comprehensive historical account, the National Institute of Neurological Disorders and Stroke offers insights into the evolution of TD recognition and diagnosis.
This knowledge propelled advancements in treating and managing TD, laying the groundwork for the nuanced care approaches we see today.
Advances in Treatment and Management
The realm of Tardive Dyskinesia (TD) has witnessed significant strides in both treatment and management, particularly with the advent of FDA-approved drugs like valbenazine and deutetrabenazine. These agents offer a ray of hope, specifically targeting the neurological pathways implicated in TD. Their introduction into the therapeutic landscape represents a paradigm shift, moving beyond symptom management to addressing the root mechanisms of the disorder.
The effectiveness of these treatments lies in their nuanced approach to dopamine modulation, a critical factor in the development of TD symptoms. By fine-tuning the levels of this neurotransmitter, patients have experienced a reduction in the involuntary movements that characterise Tardive Dyskinesia. This progress in pharmacological intervention is complemented by advancements in non-drug strategies, such as customised physical therapy programs that focus on improving motor skills and muscle control.
Understanding and mitigating the risk factors associated with antipsychotic medications have also evolved. Clinicians are now more vigilant in monitoring patients, especially those who are at a higher risk for Tardive Dyskinesia, such as the elderly and women. The adoption of newer, atypical antipsychotics, which are less likely to cause TD, is becoming more widespread, reflecting a more informed approach to prescribing practices.
For those affected by tardive dyskinesia, these advances in treatment and management have not only improved symptom control but also enhanced the overall quality of life. The journey towards better understanding and treating TD continues, with ongoing research and clinical trials paving the way for more effective interventions.
To delve deeper into the latest treatment options for Tardive Dyskinesia, the National Institute of Neurological Disorders and Stroke provides a wealth of information.
Living with Tardive Dyskinesia and its Comorbidity on mental health and movement disorders
Living with Tardive Dyskinesia (TD) is akin to navigating a relentless storm, where unpredictable gusts of involuntary movements disrupt the tranquillity of everyday life. It’s a condition that doesn’t just ripple across the surface of one’s physical well-being; it plunges deep, affecting the very essence of mental health.
The comorbidity of TD with psychiatric and movement disorders compounds the struggle, as patients grapple with the dual burden of managing their mental health condition while also battling the physical manifestations of TD. This duality is a tightrope walk between managing the symptoms of their primary mental health disorder and the side effects of the medications that treat it, often the very cause of their TD.
The psychological impact is profound, with feelings of anxiety and depression frequently accompanying the visible, uncontrollable movements. These emotional challenges are not just footnotes in the narrative of TD; they are glaring chapters that often require their own distinct therapeutic strategies.
Moreover, the social implications of TD’s physical symptoms can erode self-esteem, fueling a cycle of isolation and psychological distress. For a deeper understanding of this intersection between movement and mental health disorders, Mental Health America offers valuable insights.
The journey of those with TD is one of resilience, as they continuously adapt to the oscillations of their condition, all the while seeking a semblance of harmony between body and mind.
The Daily Reality for Individuals with tardive dyskinesia
For those living with Tardive Dyskinesia (TD), each day is marked by the unpredictable cadence of involuntary movements. Simple tasks like sipping a cup of tea or engaging in conversation can become a battleground as they wrestle with erratic facial twitches or limb spasms.
The physical aspects of TD, such as lip-smacking, grimacing, or finger writhing, are often just the tip of the iceberg. Beneath the surface, there’s a constant mental toll, with individuals hyper-aware of their uncontrollable movements, which can lead to anxiety and self-consciousness.
Social interactions can turn into a source of stress, overshadowed by the fear of judgment or misunderstanding. This can push individuals into a corner of isolation, even from loved ones who might struggle to grasp the depth of their daily challenges fully.
Employment and public activities can become daunting, as TD symptoms potentially disrupt professional tasks and draw unwanted attention. Despite the advances in treatment and understanding, the reality for those with TD is continuous navigation through a world that may not always accommodate their needs.
The journey is not just about managing a medical condition; it’s about maintaining dignity, finding supportive communities, and advocating for a life beyond the involuntary dance of Tardive Dyskinesia.
Coping Strategies and Support Systems for treatment, recovery, and maintaining health and wellness
Coping with Tardive Dyskinesia (TD) demands a multifaceted approach, where treatment is just one piece of the puzzle. Developing robust coping strategies is essential for individuals navigating the complexities of Tardive Dyskinesia. These strategies might include mindfulness techniques to reduce stress, which can exacerbate symptoms, or engaging in gentle exercises like tai chi that can improve body awareness and motor control.
Support systems play a critical role in the recovery and wellness journey. Patients need to build a network that includes healthcare professionals and peers who share the experience of living with Tardive Dyskinesia. Such community support can be found through organisations like the National Alliance on Mental Illness (NAMI), where resources and connections to others offer comfort and practical advice.
Maintaining health and wellness involves a proactive stance on treatment adherence and ensuring regular communication with doctors to fine-tune medication regimens. Patients are encouraged to advocate for themselves, staying informed about their condition and the latest treatment options.
This empowerment, combined with lifestyle adjustments prioritising mental and physical health, lays the groundwork for a more manageable life with Tardive Dyskinesia.
The Role of the FDA and Medical Community
The U.S. Food and Drug Administration (FDA) and the medical community play pivotal roles in the lives of those affected by Tardive Dyskinesia (TD). The FDA’s regulatory authority is instrumental in approving and monitoring treatments, ensuring that medications like valbenazine (Ingrezza) and deutetrabenazine (Austedo) meet stringent safety and efficacy standards. These FDA-approved treatments provide patients with options that were previously unavailable, marking a significant advancement in the management of TD.
Beyond drug approval, the FDA’s role extends to fostering patient awareness about the potential risks associated with antipsychotic medications. By mandating clear labelling and providing detailed medication guides, the FDA empowers patients and caregivers with the knowledge necessary to make informed decisions regarding their treatment plans. Meanwhile, the medical community, including physicians and mental health professionals, is responsible for translating this knowledge into practice.
Healthcare providers must ensure diligent communication with their patients, discussing the benefits and risks of antipsychotic medication and staying alert to the early signs of TD. This includes regular monitoring and, if necessary, adjusting treatment regimens to mitigate the development of TD symptoms.
The synergy between the FDA’s regulatory framework and the medical community’s clinical understanding is essential in safeguarding patients’ health while optimising therapeutic outcomes. This collaborative effort enhances the quality of care for those living with Tardive Dyskinesia.
Regulatory Approvals for TD Treatments
The FDA’s role in the battle against Tardive Dyskinesia (TD) is a beacon of hope for patients seeking relief from this challenging condition. With the regulatory approval of valbenazine (Ingrezza) and deutetrabenazine (Austedo), the landscape of TD treatment has been transformed, offering new avenues for symptom management.
These medications, specifically designed to address the dopamine receptor sensitivity that underpins TD, have undergone rigorous clinical trials to demonstrate their safety and effectiveness. It’s through this meticulous process that the FDA has provided the green light, setting a precedent for future therapeutic innovations in the realm of movement disorders.
Patients and healthcare providers now have access to treatments that are not just experimental but backed by the assurance of regulatory scrutiny. This stamp of approval is more than a bureaucratic milestone; it’s a critical layer of protection for patients navigating the complex world of medication management.
For those interested in the full scope of the FDA’s involvement in TD treatments, the National Institute of Neurological Disorders and Stroke offers an in-depth look.
The FDA’s commitment to rigorous evaluation ensures that the treatments reaching patients are not only effective, but also meet the highest standards of care.
The Importance of Patient Awareness and Doctor-Patient Communication

In Tardive Dyskinesia (TD), patient awareness and doctor-patient communication are pivotal to effective treatment. Knowledge empowers patients, enabling them to recognise early symptoms and understand the risks associated with their medications.
This awareness is crucial, as TD can manifest subtly before progressing to more pronounced and potentially disabling movements. Patients can actively participate in their treatment plans when informed, voicing concerns and preferences that might otherwise go unheard.
On the other hand, doctor-patient communication is the bridge that connects medical expertise to patient experience. Through open dialogue, doctors can tailor treatment, considering the unique aspects of each patient’s condition.
Moreover, effective communication ensures that patients are not left in the dark about the potential side effects of antipsychotics, a common cause of TD. It’s a shared journey where both parties must navigate the complexities of treatment options, side effect management, and long-term care strategies.
In fostering a collaborative environment, doctors can encourage adherence to treatment while patients maintain agency over their health outcomes. For a deeper dive into the critical role of patient-doctor communication in managing Tardive Dyskinesia, the National Alliance on Mental Illness (NAMI) offers extensive resources. This synergy is not just beneficial; it’s essential for the successful management of Tardive Dyskinesia.
Tardive dystonia vs Tardive Dyskinesia
Tardive dyskinesia (TD) and tardive dystonia are both movement disorders associated with the long-term use of antipsychotic medications, but they present with distinct characteristics. TD is primarily characterised by repetitive, involuntary movements, particularly of the lower face and jaw, including lip-smacking, tongue protrusion, and grimacing. These quick, jerky movements can also affect the extremities and trunk, often leading to social discomfort and functional impairment.
Tardive dystonia, on the other hand, involves sustained muscle contractions resulting in twisting and repetitive movements or abnormal postures. These can be painful and affect any part of the body, including the neck (cervical dystonia), limbs, or trunk, leading to significant disability. Unlike the rapid movements of TD, tardive dystonia’s contractions are often slower and can be sustained, which can cause persistent abnormal postures or positions.
Both conditions are linked to the prolonged blockade of dopamine receptors by antipsychotic drugs, yet they differ in their clinical management and treatment approaches. Understanding the nuances between these two forms of tardive syndromes is crucial for accurate diagnosis and appropriate treatment. While there are medications and therapies available to manage symptoms, the complexities of these disorders underscore the importance of careful medication monitoring and informed patient care.
Navigating the complexities of Tardive Dyskinesia (TD) requires awareness, understanding, and a proactive approach to treatment. With the FDA’s approval of targeted medications, patients have more tools to manage involuntary movements and improve their quality of life. Remember, TD’s journey is unique to each individual, and with the right support and care, life can still be lived to its fullest. For more information and resources on managing TD, visit NAMI. Take that first step towards managing your health today.
Parkinsonian with Tardive dystonia and Dyskinesia
In the complex spectrum of movement disorders, the overlap between Parkinsonian symptoms, tardive dystonia, and TD presents unique challenges. Parkinsonian symptoms, often characterised by bradykinesia, rigidity, and tremors, can sometimes be confused with the movement irregularities seen in Tardive Dyskinesia. Tardive dystonia, with its sustained muscle contractions and abnormal postures, adds another layer to the diagnostic puzzle.
Understanding the distinctions and connections between these conditions is vital for effective management and treatment. For a more detailed exploration of these movement disorders, WebMD provides an insightful overview.
It’s crucial for patients and healthcare providers to recognise the nuances of each condition to ensure accurate diagnosis and tailored treatment plans.
Conclusion
Tardive dyskinesia is a neurological disorder characterised by involuntary movements, commonly affecting the face and limbs. The exact causes of tardive dyskinesia are not fully understood, but it is believed to be a side effect of long-term use of certain medications, particularly antipsychotics.
Symptoms can vary in severity and may include repetitive facial grimacing, tongue thrusting, and rapid movements of the arms or legs. It is important to note that tardive dyskinesia can be distressing for those affected, as it can interfere with daily activities and social interactions.
Treatment options for tardive dyskinesia include adjusting medication dosages or switching to alternative medications that have a lower risk of causing these symptoms.
Additionally, certain medications, such as valbenazine and deutetrabenazine, have been approved by the FDA specifically for the treatment of tardive dyskinesia.
It is crucial for individuals experiencing symptoms of tardive dyskinesia to consult with their healthcare provider for proper diagnosis and management strategies.
Popular Questions
How do you fix tardive dyskinesia?
Tardive dyskinesia is a neurological disorder that causes involuntary movements in the body. These repetitive movements often affect the face, tongue, and limbs.
The exact cause of tardive dyskinesia is not fully understood, but it is believed to be related to the long-term use of certain medications, particularly antipsychotics. Antipsychotics are commonly prescribed for conditions such as schizophrenia and bipolar disorder.
The symptoms of tardive dyskinesia can vary from person to person, but they typically include twitching, grimacing, and tongue protrusion. It is important to note that tardive dyskinesia may not appear until months or even years after starting medication.
Treatment options for tardive dyskinesia include adjusting or discontinuing the medication causing the symptoms, as well as using other medications to manage the movements. Additionally, therapies such as speech therapy and physical therapy may also be beneficial in managing the symptoms of this condition.
It is important for individuals who are taking antipsychotic medications to be aware of the potential risk of developing tardive dyskinesia and to discuss any concerns with their healthcare provider.
- Drugs on prescription: At the moment, the only drug licensed for treating TD is tetrabenazine. It’s a drug used to treat movement disorders. However, common side effects of this drug include Parkinsonism, anxiety and depression, so you may want to think carefully before considering this option.
What aggravates tardive dyskinesia?
Tardive dyskinesia is a neurological disorder that is characterised by involuntary, repetitive movements of the mouth, face, and other body parts. It is believed to be caused by long-term use of certain medications, such as antipsychotics.
The exact mechanism behind the development of tardive dyskinesia is not fully understood, but it is thought to involve changes in dopamine receptors in the brain. Symptoms of tardive dyskinesia can vary widely from person to person and may include lip-smacking, tongue protrusion, grimacing, and rapid eye blinking. These movements can sometimes be severe and interfere with daily activities.
Treatment options for tardive dyskinesia include:
- Reducing or discontinuing the use of the offending medication.
- Switching to a different medication that has a lower risk of causing tardive dyskinesia.
- Using medications that target specific symptoms.
- Movement disorders like tardive dyskinesias are frequently aggravated by the use of drugs that block dopamine. In susceptible patients, even a single dose of an anti-dopaminergic medicine can quickly develop disabling movement disorders.
What is the drug of choice for tardive dyskinesia?
Tardive dyskinesia is a neurological disorder that is characterised by repetitive and involuntary movements of the face, tongue, and other body parts. The exact cause of this condition is still not fully understood, but it is believed to be related to the long-term use of certain medications, particularly antipsychotics.
These medications work by altering dopamine levels in the brain, which can lead to abnormal movements over time. The symptoms of tardive dyskinesia can vary from person to person but commonly include facial grimacing, rapid eye blinking, lip-smacking, and jerking movements of the limbs. Although there is no cure for tardive dyskinesia, there are treatment options available to help manage the symptoms.
These may include adjusting medication dosages or switching to alternative medications with lower risk of causing tardive dyskinesia. In some cases, additional medications or therapies such as botulinum toxin injections or deep brain stimulation may be recommended.
It is important for individuals experiencing these symptoms to consult with their healthcare provider for proper diagnosis and management.
- Other than ceasing or switching antipsychotic medication, the strongest current evidence for TD treatment is the use of the VMAT inhibitors, deutetrabenazine and valbenazine
How can tardive dyskinesia be diagnosed?
Tardive Dyskinesia is a neurological disorder characterised by involuntary, repetitive movements of the face and body. It is most commonly caused as a side effect of long-term use of certain psychiatric medications, such as antipsychotics.
The exact cause of Tardive Dyskinesia is still not fully understood, but it is believed to be related to the dopamine receptors in the brain. Symptoms can range from mild to severe, and may include grimacing, lip smacking, tongue protrusion, and jerking movements of the limbs. These movements can be embarrassing and distressing for individuals affected by Tardive Dyskinesia, leading to social isolation and decreased quality of life.
Treatment options for this condition include medication adjustments or discontinuation, as well as the use of medications specifically designed to target the symptoms of Tardive Dyskinesia. In some cases, physical therapy or occupational therapy may also be beneficial in managing the symptoms. It is important for individuals experiencing these symptoms to seek medical attention for an accurate diagnosis and appropriate treatment plan.
What is Dyskinesia
Dyskinesia refers to an abnormal, involuntary movement disorder that can affect individuals in various ways. There are several types of dyskinesia, including tardive dyskinesia, which can be a side effect of certain medications used to treat mental illnesses such as schizophrenia or bipolar disorder.
Additionally, there is also primary dyskinesia, which is usually a genetic or hereditary condition. In terms of treatment, it is crucial for individuals experiencing dyskinesia to consult with a healthcare professional or specialist who can diagnose and provide appropriate care. Treatment options vary depending on the type and underlying cause of dyskinesia. Medications such as anti-Parkinsonian drugs or botulinum toxin injections can sometimes help manage the symptoms of dyskinesia.
Other options may include physical therapy, speech therapy, or even deep brain stimulation in severe cases.
It’s important to note that dyskinesia can have a significant impact on an individual’s quality of life, so seeking professional help and support is essential. It’s also important to educate oneself and raise awareness about dyskinesia to promote understanding and eliminate stigmas around these movement disorders.
What is bradykinesia
Bradykinesia is a medical term used to describe a symptom characterised by slow movement and a decrease in spontaneous muscle activity. It is most commonly associated with neurological disorders such as Parkinson's disease.
The condition occurs due to a dysfunction in the basal ganglia, a part of the brain responsible for controlling movement. This dysfunction leads to a decrease in the production of dopamine, a neurotransmitter that plays a crucial role in coordinating movement.
As a result, individuals with bradykinesia tend to have difficulties initiating and executing movements, leading to a slowness in their overall motor skills. Other symptoms often associated with bradykinesia include muscle stiffness, rigidity, and tremors.
What are antipsychotics prescribed for
Antipsychotics are medications primarily prescribed to treat and manage various mental health conditions, particularly psychotic disorders like schizophrenia and bipolar disorder. These medications work by balancing certain chemicals in the brain known as neurotransmitters, such as dopamine and serotonin.
Antipsychotics are effective in reducing or eliminating symptoms associated with psychosis, including hallucinations, delusions, disorganized thinking, and agitation. They are also used to stabilize mood and treat symptoms of mood disorders like bipolar disorder, provide relief for individuals experiencing severe anxiety or insomnia, and can sometimes be used as a component of treatment for depression that has not responded to other medications.
It is important to note that antipsychotics are typically prescribed as part of a comprehensive treatment plan that may also include therapy, lifestyle modifications, and other interventions.
The specific type, dosage, and duration of antipsychotic medication can vary depending on the individual's diagnosis, symptoms, and response to treatment. It is essential to work closely with a healthcare professional when taking antipsychotics to ensure proper monitoring and management of any potential side effects or adverse reactions.
Sources
- 1.https://www.webmd.com/mental-health/tardive-dyskinesia
- 2.https://www.ninds.nih.gov/health-information/disorders/tardive-dyskinesia
- 3.https://my.clevelandclinic.org/health/diseases/6125-tardive-dyskinesia
- 4.https://emedicine.medscape.com/article/1151826-overview
- 5.https://medlineplus.gov/ency/article/000685.htm
- 6.https://www.nami.org/About-Mental-Illness/Treatments/Mental-Health-Medications/Tardive-Dyskinesia
- 7.https://www.mind.org.uk/information-support/types-of-mental-health-problems/tardive-dyskinesia-td/about-tardive-dyskinesia/
- 8.https://rarediseases.org/rare-diseases/tardive-dyskinesia/
- 9.https://en.wikipedia.org/wiki/Tardive_dyskinesia
