Understanding Obsessive-Compulsive Disorder: A Comprehensive Guide
Lesson 16
Obsessive-compulsive disorder (OCD) is a complex psychiatric illness that can wreak havoc on the lives of those it afflicts. Characterised by intrusive, anxiety-provoking thoughts and repetitive behaviours aimed at reducing the associated anxiety or worry, and the disorder is often profoundly misunderstood.
This section will provide an informative overview of OCD, delving into its prevalence, symptoms, causes, and treatments. We will examine how understanding of OCD has evolved over time and highlight vital scientific insights that shed light on the biological basis of the disorder. While Obsessive-compulsive disorder certainly poses challenges, knowledge and compassion are powerful tools in confronting this condition. There are many reasons for hope when it comes to living well with OCD.
Table of Contents
- Key Takeaways
- Essential Facts and Figures about OCD
- Prevalence of OCD in the United States
- Age and Gender Distribution of OCD
- Defining OCD: Obsessions and Compulsions
- Causes and Symptoms of OCD
- Impact of OCD on Daily Life
- Historical Perspective on OCD
- Recognition of OCD as a Psychiatric Disorder
- Evolution of Theories and Treatments for OCD
- Statistical Insights into OCD
- Age of Onset and Gender Equality in OCD
- Genetic Factors and Cultural Prevalence of OCD
- Comparing OCD with Other Disorders
- Differences between OCD and OCPD
- Misconceptions about OCD
- Scientific Findings on OCD
- Brain Imaging Studies and OCD
- Neurotransmitter Abnormalities in OCD
- Pure O form of OCD
- Moral Scrupulosity Form of OCD
- Paedophilia OCD (pOCD)
- Religious obsessions in Obsessive-Compulsive Disorder (OCD)
- Perinatal obsessive-compulsive disorder
- Sexual orientation obsessions in OCD
- Misconceptions about OCD
- Comparing OCD with Other Disorders
- Differences between OCD and OCPD
- Disorders related to OCD
- Body dysmorphic disorder (BDD)
- Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS)
- Body Focused Repetitive Behaviours (BFRBs)
- Olfactory Reference Syndrome (ORS)
- Misophonia
- Mistaken for OCD
- Tourette Syndrome
- Impulse control disorders
- Autism Spectrum Disorders
- Psychotic disorders
Key Facts
- Lifetime prevalence of OCD affects approximately 2-3% of people in the United States, with 1 in 40 adults and 1 in 100 children being affected.
- OCD is a mental disorder characterised by obsessions (intrusive thoughts) and compulsions (repetitive behaviours).
- The cause of obsessive-compulsive disorder is unknown, but it likely involves a combination of biological and environmental factors.
- OCD symptoms can cause significant distress and impairment in daily functioning.
- OCD was first recognised as a psychiatric disorder in the 19th century, and has since evolved in terms of theories and treatments.
- Compulsions are done to reduce anxiety or suppress or neutralise the distress by preventing a feared outcome (compulsive rituals).
- Recurrent, unwelcome thoughts, images, ideas or doubts, (obsessions)
- Experience significant problems and functional impairment in daily life due to these thoughts or behaviours.
- Many adults with OCD recognise that their compulsive behaviours do not make sense.
- There is no cure for OCD, treatments help people manage their symptoms, engage in daily activities, for a full, active life.
- OCD is the fourth most common mental disorder after depression, alcohol and substance misuse, and social phobia with a lifetime prevalence.
- OCD is a disabling disorder that is twice as common as schizophrenia.
Definition: Obsessive-compulsive disorder (OCD) is often a long-lasting disorder in which a person has uncontrollable, reoccurring thoughts (obsessions), and behaviours (compulsions) that he or she feels the urge to repeat over and over.
Essential Facts and Figures about OCD and Overview

Obsessive-compulsive disorder (OCD) is a surprisingly common psychiatric condition, affecting around 2-3% of the population in the United States. This equates to over nine million American adults dealing with OCD. The disorder generally emerges in adolescence or early adulthood, though onset can occur in childhood.
Evidence indicates boys are more prone to developing OCD at a young age, the earliest age recorded in literature is four or five.
Studies have looked at the prevalence of Attention-deficit/hyperactivity disorder (ADHD) in Obsessive-compulsive disorder (OCD) populations, and estimate that approximately 30% of patients with OCD also have ADHD.
Obsessive-compulsive disorder symptoms typically include the presence of both unwanted obsessions and compulsions. However, some individuals experience obsessive thoughts or just compulsive behaviours.
A compulsion can either be overt and observable by others, such as checking that a door is locked, or a covert mental act that cannot be observed, such as repeating a certain phrase in one's mind.
The leading habits revolve around contamination, a fear of things that might be dirty or a having a compulsion to clean (you may hear this called "obsessive cleanliness disorder") with the fears of causing harm, the need for order/symmetry, and taboo thoughts related to sex, religion, or violence.
Don’t get pleasure from their compulsions, but may feel temporary relief from their anxiety.
Other points to consider, individuals with OCD have generally been shown in research to have this inflated feeling of responsibility, and they often sense that they are going to be responsible for something terrible that could happen or if they fail to do something, they will be liable for that harm too. So, they naturally have slightly higher levels of fear of guilt, making them more susceptible to indecisiveness.
This indecisiveness leads to difficulty terminating an action as well as evoking doubt whether an action was done properly, which leads to repetition of that action once again.
Common compulsions include:
- Excessive cleaning and handwashing.
- Checking behaviours.
- You are repeating routine activities.
- Mental rituals like counting or praying.
While OCD has likely existed throughout history, it was not formally recognised as a distinct psychiatric disorder until the 19th century. Today, OCD is considered a chronic and long-lasting condition. However, the severity of symptoms can fluctuate over time. With proper treatment and management, many people with OCD can live fulfilling lives and experience periods of remission. However, they often find it embarrassing or distressing to talk about, and feel guilty or ashamed for having such thoughts and rituals.
Prevalence of OCD in the United States
Obsessive-compulsive disorder (OCD) is a surprisingly common psychiatric condition in the United States, with prevalence estimates ranging from 1.6% to 2.3% of the general population. This equates to over 9 million American adults dealing with OCD. To put that staggering figure in perspective, OCD is more prevalent than bipolar disorder or schizophrenia.
According to the National Institute of Mental Health (NIMH), approximately 1 in 40 U.S. adults and 1 in 100 U.S. children currently have an Obsessive-compulsive disorder. While OCD can develop at any age, studies indicate around half of all cases emerge in childhood or adolescence. The average age of onset is 19 years old. However, males often develop OCD at a younger age than females.
It’s estimated that about 12 in every 1,000 people in the UK are affected by OCD, which means more than 750,000 people in the UK. (Mind) – and inquiries to the Priory for private mental health treatment for Obsessive Compulsive Disorder have more than doubled in the last year.
OCD appears to impact all ethnic and racial groups equally. However, identifying OCD can be challenging in minority populations where mental health resources are limited and stigma persists. Boosting awareness and access to care is critical to supporting those with OCD from all backgrounds.
While OCD certainly poses challenges, recovery is absolutely possible. With increased understanding and compassion, those with OCD can find the help they need to manage symptoms and reclaim their lives. As awareness grows, no one needs to suffer alone. There are many reasons for hope when it comes to living well with OCD.
Age and Gender Distribution of OCD
Obsessive-compulsive disorder (OCD) frequently emerges during childhood or adolescence, though it can develop at any age. Research indicates around 50% of individuals experience their first OCD symptoms before age 20.
The average age of onset is 19 years old for both males and females.
Symptoms generally first appear in late adolescence for men and the early 20s for women.
However, studies show males often develop OCD at a younger age compared to females.
The reasons for earlier onset in males remain unclear.
One theory suggests hormones like testosterone may influence brain development in ways that increase OCD vulnerability.
Differences in symptom expression could also play a role. For instance, males exhibit higher rates of symmetry/ordering obsessions and repeating rituals, which may be more observable at a young age.
In contrast, females tend to have more internal obsessions like taboo thoughts, which could go unnoticed longer. While the gender gap in age of onset is well-documented, overall Obsessive-compulsive disorder prevalence is equal among adult males and females.
Understanding age and gender patterns provides insight into OCD risk factors. But regardless of demographics, compassionate support is essential for anyone struggling with this disorder.
Defining Obsessive-Compulsive disorder : Obsessions and Compulsions
Obsessive-compulsive disorder affects approximately 1-3% of people, making it a relatively common disorder.
However, OCD is frequently misunderstood by the public.
Learning the facts about OCD is the first step in fostering compassion and support for those dealing with this challenging condition.
Obsessive-compulsive disorder (OCD) is characterised by two core symptoms - obsessions and compulsions. Understanding the distinction between these two manifestations of OCD is critical to comprehend the condition properly.
Obsessions are recurring, persistent, and intrusive thoughts, urges, or images that trigger intense anxiety. Individuals experiencing those distressing thoughts, known as obsessions, engage in behavioural or "Acts of the mind", referred to as compulsions. They are unwanted and often disturbing in essence. Everyone sometimes have intrusive thoughts, and it is our reaction to those intrusive thoughts that define OCD. ("Acts of the mind" alleviating oneself of intrusive thoughts and uncomfortable feelings).
Compulsions are repetitive behaviours or mental acts that OCD sufferers feel driven to alleviate oneself of intrusive thoughts and uncomfortable feelings in response to an obsession. Then we do rituals, which reinforces in our brains that the only way we survived having those thoughts was to do compulsions. Motivating the individual to continue with the compulsive cycle of hell.
Common obsessions revolve around themes of:
- Contamination - excessive fears of germs, toxins, bodily fluids
- Doubts - repetitive doubts about having made mistakes, such as forgetting to lock a door or accidentally harming others
- Order - distress when objects are not orderly or symmetrical
- Taboo thoughts - forbidden or perverse sexual, religious, or violent thoughts
Obsessions are ego-dystonic, meaning they feel alien and cause significant distress. The individual recognises that the obsessions are irrational or excessive.
To reduce the anxiety or mental discomfort triggered by obsessions, people with OCD feel compelled to perform compulsions - repetitive behaviours or mental acts.
Common compulsions include:
- Excessive cleaning/handwashing
- Checking behaviours, such as repeatedly checking that a door is locked
- Counting/arranging items until it feels “just right.”
- Mental rituals like silently reciting phrases or prayers
Excessive cleaning/handwashing (obsessive cleanliness disorder) people with this disorder often feel intense distress when they perceive a potential source of contamination, even if it is minimal or unlikely to cause them or others harm. They may constantly wash their hands, disinfect their surroundings, or avoid touching objects or people they perceive as unclean.
Individuals have an overwhelming fear of contamination or germs, which drives them to engage in compulsive cleaning rituals to alleviate their anxiety. Therefore, compulsions provide only temporary relief from their anxiety.
Unfortunately, the cycle tends to reinforce itself - the more someone performs a compulsion, the stronger the urge becomes. This leads to a self-perpetuating pattern that can severely disrupt daily functioning.

Jessica Alba actress has said in a 2012 interview with Allure Magazine, that she suffers from OCD and is a “germaphobe”. She washes her hands constantly and that she is very careful about what she touches.
Alba also said that she has to be in control of everything in her life, or she feels like she will “lose it.” Alba's early life was marked by a multitude of physical maladies.
During childhood, she suffered from pneumonia four to five times a year and had partially collapsed lungs twice, as well as a ruptured appendix and tonsillar cyst.
She has also had asthma since she was a child She became isolated from other children at school because she was hospitalised so often, no one knew her well enough to befriend her.
Streptococcus can lead to various physical illnesses. One common illness is strep throat, where the bacteria infect the throat and tonsils, causing symptoms such as sore throat, difficulty swallowing, and swollen lymph nodes.
Additionally, streptococcal pneumonia is a respiratory infection that can lead to coughing, difficulty breathing, and chest pain. In severe cases, this infection can even result in pneumonia, which she had on a number of occasions.
Causes and Symptoms of OCD
The exact causes of OCD are not fully understood, but a combination of genetic, environmental, and neurobiological factors such as brain structure and functioning, and neurotransmitter abnormalities are believed to contribute to its development.
Genetic factors play a role in OCD, as studies have shown that individuals with a family history of OCD are more likely to develop the disorder themselves. Certain genes related to serotonin and dopamine regulation have been implicated in OCD.
Neurobiological factors also play a role, as there are abnormalities in certain brain regions and neurotransmitter systems involved in OCD. The brain regions implicated include the orbitofrontal cortex, anterior cingulate cortex, and the basal ganglia. Dysregulation of serotonin, dopamine, and glutamate neurotransmitters have also been observed in individuals with OCD.
Environmental factors such as childhood trauma, stress, and infections have been associated with the development of OCD. Traumatic experiences or significant life events may trigger or worsen symptoms in individuals predisposed to the disorder.
Common compulsions include excessive handwashing or cleaning, repeated checking, counting, arranging or organizing, and seeking reassurance.
Stressful life events can also play a role in triggering onset. OCD symptoms typically cause significant distress and impairment in daily functioning. However, with proper treatment, many individuals can achieve remission for periods and live fulfilling lives.
Understanding obsessions and compulsions is the foundation for recognising OCD. Insight into this cycle enables more effective management of the disorder. With compassionate support, those with OCD can break free from the grip of relentless obsessions and compulsions.
Temperament: Some research suggests that individuals who are more reserved and experience negative emotions as children may have a higher likelihood of developing OCD. These individuals may also exhibit symptoms of anxiety and depression.
Children who suddenly develop OCD symptoms or experience a worsening of OCD symptoms after a streptococcal infection may be diagnosed with Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS).
Impact of Obsessive-compulsive disorder on Daily Life
Obsessive-compulsive disorder (OCD) can have a profoundly detrimental impact on daily functioning and quality of life. The relentless cycle of intrusive thoughts and anxiety-reducing rituals consumes mental energy and time, often crowding out essential activities. OCD commonly leads to social isolation, strained relationships, lost productivity at work or school, and an overall diminished ability to enjoy life.
For many with OCD, simple tasks become arduous ordeals. Getting ready in the morning can take hours if rituals like showering or handwashing spiral out of control. Rigid routines make it hard to adapt to changes in schedule or environment.

In The Netflix documentary about David Beckham’s personal life, the 48-year-old former footballer star talks about his “tiring” OCD, which sees him spending hours cleaning the house after his family has gone to bed.
His OCD causes him to have everything in “perfect symmetry.”
He said that his OCD is something that he has always had to deal with and that it is a part of his life.
The debilitating nature of OCD may prevent some people from working, attending school, leaving the house, or maintaining relationships.
They may give up hobbies they once enjoyed. A study found that 50% of individuals with OCD experience severe impairment in daily functioning.
OCD rituals also take a toll on family members who accommodate them. Loved ones often struggle to help those with OCD break free from the prison of their compulsions.
Some may grow frustrated and distant. OCD has been linked to increased rates of unemployment, divorce, and financial difficulties.
However, with compassionate understanding and proper treatment, the grip of OCD can be overcome.
Recovery allows for rebuilding life on a new, healthy foundation. They may first have to overcome the first barrier, often ashamed and embarrassed by their condition finding it very difficult to discuss their symptoms with healthcare professionals, friends, family or carers.
Recognition of OCD as a Psychiatric Disorder
Obsessive-compulsive disorder (OCD) has likely existed for centuries, yet recognition of OCD as a distinct psychiatric illness separate from other conditions was surprisingly recent. While OCD symptoms were described in ancient religious texts, OCD was not recognised as a medical disorder until the 19th century, when French neurologist Jean-Martin Charcot first classified it as a neurological entity named “obsessive neurosis.”
This pivotal development marked the first formal identification of OCD as its own disorder. However, it would take another century before the term “obsessive-compulsive disorder” first appeared in the Diagnostic and Statistical Manual of Mental Disorders (DSM-III) in 1980, finally cementing OCD as a distinct psychiatric illness in the medical community.
Before 1980, OCD was lumped under broader categories like “neurosis” or “anxiety neurosis.” The inclusion of obsessive-compulsive disorder as its own diagnosis in the DSM-III enabled focused research into the biological and behavioural underpinnings of OCD. It was paving the way for new treatments targeting the specific symptoms and mechanisms of OCD.
While OCD has likely caused distress since ancient times, recognition of OCD as a valid psychiatric disorder only occurred within the last 140 years.
This formal medical classification was critical to understanding the unique characteristics of OCD compared to other mental illnesses.
Dedicated research into OCD has led to significant advances, providing hope to the millions afflicted by debilitating obsessive thoughts and compulsive rituals.
Evolution of Theories and Treatments for OCD
Historical Perspective on OCD
Obsessive-compulsive disorder (OCD) has likely existed throughout history, yet recognition of OCD as a distinct psychiatric illness is surprisingly recent. Understanding how perceptions of OCD evolved over-time provides insight into this complex condition.
Understanding of obsessive-compulsive disorder (OCD) and approaches to treating it have evolved considerably over the past century.
Early psychoanalytic theories emphasised unconscious conflicts, while later behavioural models focused on learned habits. Pioneering medications and therapies in the 1960s and 1970s paved the way for today’s multimodal treatment.
In the early 1900s, psychoanalysis linked OCD to unresolved unconscious issues from childhood, often related to toilet training or sexuality. This view persisted for decades until behavioural theories emerged in the 1960s.
Researchers like Victor Meyer conceptualised OCD as a learned disorder fuelled by the short-term relief provided by compulsions.
The first medications to effectively treat obsessive-compulsive disorder were the tricyclic antidepressants clomipramine and imipramine, introduced in the 1970s. Stanley Rachman and Isaac Marks developed around the same time, pioneering cognitive-behavioural therapy (CBT) techniques to address maladaptive thoughts and behaviours.
Today, the gold standard for OCD treatment is a combination of CBT with medications like selective serotonin reuptake inhibitors (SSRIs). As scientific understanding of OCD continues to evolve, more targeted and effective therapies will undoubtedly emerge. However, the breakthroughs of the 1960s and 1970s laid the groundwork for modern treatment.
Psychotherapy can be an effective treatment for adults and children with OCD.
Research shows that certain types of psychotherapy, including cognitive behavioural therapy and other related therapies, can be as effective as medication for many people. For others, psychotherapy may be most effective when combined with medication.
Cognitive Behavioural Therapy called Exposure and Response Prevention (ERP), Acceptance and Commitment Therapy (ACT) and Inference-Based CBT (I-CBT) all of which research has shown to be very beneficial for many patients.
Exposure and response prevention (ERP) is considered the most effective treatment for all forms of OCD.
Concerns about moral aspects of exposure may arise, as it might seem that engaging in certain actions could lead to immoral behaviour or unforeseen consequences. It is important to note that exposure for the fear of lying does not necessarily involve lying itself, but rather engaging in behaviours where it is unclear if a lie occurred or the significance of a partial truth is unknown.
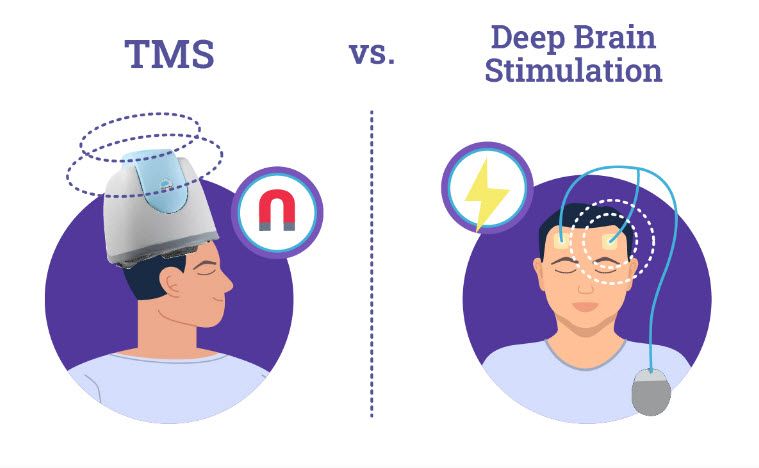
Deep Brain Stimulation (DBS) involves the stimulation of chronically implanted electrodes deep in the brain, and targeting the NAc core, it is FDA approved for treating Parkinson’s Disease, a neurodegenerative disease affecting the dopamine neurons in the striatum and sub-thalamic nucleus to alleviate Parkinsonian motor deficits. Neuromodulation with DBS often restores motor function in these patients, permitting many to live much improved lives.
It is also being explored as treatments for treatment-resistant depression, Obsessive-Compulsive Disorder, addiction, and other neurological and psychiatric issues.
FDA has approved using DBS to treat severe cases of OCD under a Humanitarian Device Exemption. This exemption allows the use of a medical device, such as DBS, for rare diseases or conditions that affect a relatively small number of people, making it challenging to gather enough evidence to establish the device’s effectiveness.
Deep Transcranial Magnetic Stimulation, or Deep TMS™, has been shown to safely and effectively alleviate the symptoms of obsessive-compulsive disorder (OCD), particularly those patients who have not achieved sufficient improvement from traditional OCD treatment options.
In 2018, the FDA approved using a deep form of repetitive transcranial magnetic stimulation (rTMS)—along with medication, psychotherapy, or a combination of both—to treat people with severe OCD who did not respond to other treatments.
In 2022, this approval was extended to standard TMS devices.
Health care providers can prescribe medication to help with OCD. The most common medications for OCD are antidepressants that target serotonin. Serotonin is a chemical in the brain related to depression and OCD. The largest category of antidepressants is known as selective serotonin reuptake inhibitors.
Antidepressant treatment can take 8–12 weeks before symptoms begin to improve, and treatment for OCD may require higher doses than are typically used to treat depression.
They include fluvoxamine (Luvox), sertraline (Zoloft), citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac), and paroxetine (Paxil). They can help by boosting serotonin levels in the brain.
For general information on mental health and to locate treatment services in your area, call the Substance Abuse and Mental Health Services Administration (SAMHSA) Helpline at 1-800-662-HELP (4357).
Transcranial Magnetic Stimulation (TMS) is a noninvasive treatment with lower risks and complications compared to Deep Brain Stimulation (DBS). It is supported by scientific studies and FDA approval. TMS is typically recommended for patients dealing with treatment-resistant depression, OCD, or anxiety, who would like minimal disruption to their daily life.
Cannabis Smoking
Individuals with obsessive-compulsive disorder report that the severity of their symptoms declined by almost half within four hours of smoking cannabis, according to a Washington State University study.
Patients reported:
- A 60% reduction in compulsions
- 49% reduction in intrusions
- 52% reduction in anxiety from before to after inhaling cannabis
The study, recently published in the Journal of Affective Disorders, also found that higher doses and cannabis with higher concentrations of CBD, or cannabidiol, were associated with larger reductions in compulsions.
Carrie Cuttler – Washington State University said "The CBD findings are really promising because it is not intoxicating".
Key Statistical Insights into OCD
Obsessive-compulsive disorder (OCD) affects approximately 1-3% of the population, with an average age of onset around 19 years old. While OCD can develop at any age, half of all cases emerge by early adulthood. Intriguingly, some key statistical patterns have emerged that provide insight into OCD risk factors.
Studies have looked at the prevalence of Attention-deficit/hyperactivity disorder (ADHD) in Obsessive-compulsive disorder (OCD) populations and estimate that approximately 30% of patients with OCD also have ADHD.
Age of Onset and Gender Equality in OCD
Research shows that obsessive-compulsive disorder (OCD) frequently begins in childhood or adolescence, though it can develop at any age. On average, males tend to experience onset of OCD symptoms about 3–5 years earlier than females. However, by adulthood, OCD is seen at nearly equal rates in men and women.
Several theories may explain the earlier age of onset in males:
- Changes in hormones like testosterone during puberty could influence brain development in ways that increase OCD vulnerability in males.
- Differences in symptom type - males exhibit higher rates of symmetry obsessions and repeating rituals, which may be observable sooner in childhood.
- Females tend to have more hidden internal obsessions, like taboo thoughts that go unnoticed for longer.
- Gender norms may make it more acceptable for younger males to display certain OCD behaviours publicly, while females may feel pressure to hide symptoms.
However, while statistics show this gender gap in age of onset, OCD can develop at any time and does not discriminate between
genders. Approximately half of all OCD cases emerge by early adulthood in both males and females.
Understanding subtle gender patterns provides insight, but compassionate support is vital for anyone struggling with OCD regardless of age or
gender. While the onset may differ, the inner experience is one of anxiety and suffering. With empathy and care, those with OCD can find the help they need to manage this challenging disorder.
Regardless of age or gender, compassion and support are vital for anyone struggling with this disorder. While statistics reveal trends, OCD can develop at any time and does not discriminate.
Genetic Factors and Cultural Prevalence of OCD
Research has shown that obsessive-compulsive disorder (OCD) has a strong genetic component and often runs in families. If you have a first-degree relative, such as a parent or sibling, with OCD, your risk of developing the disorder is elevated. However, no single “OCD gene” has been identified. Instead, many variations in different genes likely contribute to one’s susceptibility.
However, many neurological diseases are impacted by strongly acting mutations which can cause disease by themselves, says David Goldstein, PhD, director of the Institute for Genomic Medicine at Columbia. New evidence has shown a strong correlation between OCD and rare mutations, particularly in a gene called SLITRK5 that had been previously linked to OCD in candidate-gene studies.
While genetics play a role, environmental factors often serve as triggers that activate OCD in predisposed individuals. Stressful or traumatic life events are frequently quoted as precipitating factors. Ultimately, OCD likely arises from a complex interplay between biological vulnerabilities and external stressors.
Interestingly, epidemiological studies reveal that OCD occurs globally with similar prevalence rates across diverse cultures and ethnicities. This consistent cross-cultural pattern implies biological factors substantially influence OCD risk, since genetics are universal while social factors differ between populations.
However, cultural context may shape how OCD manifests. For example, some studies note religious obsessions are more common in devout cultures. Other research suggests collectivist cultures have lower OCD prevalence, possibly due to more assertive family support systems. Nevertheless, the core experience of anxiety and obsessive thinking remains consistent worldwide.
While genes may increase vulnerability, they do not seal one’s fate.
Through compassionate understanding and evidence-based treatment methods, unfortunately, OCD is not curable, but those with OCD can gain control over this biologically-based yet treatable disorder. Environmental influences and individual empowerment can overcome genetic odds.
Scientific Findings on OCD
Obsessive-compulsive disorder (OCD) has been considerably studied by researchers seeking to uncover the underlying biological and psychological mechanisms of this complex condition. Modern scientific investigations provide insight into the neurological underpinnings and psychological factors driving OCD.
Brain Imaging Studies and OCD

Modern brain imaging techniques have provided fascinating insights into the underlying neurological basis of obsessive-compulsive disorder (OCD). Sophisticated imaging modalities like functional magnetic resonance imaging (fMRI) and positron emission tomography (PET) have revealed intriguing differences in the brains of OCD patients compared to healthy individuals.
These discoveries shed light on the biological mechanisms that may drive the unwanted, anxiety-provoking thoughts and compulsive rituals characteristic of this psychiatric condition.

The actor Leonardo DiCaprio has shared in a 2014 interview that he has OCD and performs daily "rituals". He has always dealt with OCD and considers it a part of his life.
To keep his OCD under control, DiCaprio stays active by working out and staying busy.
Other celebrities have also found ways to manage their OCD and live successful lives.
Each person's experience with OCD is unique, but these celebrities serve as examples that it is possible to overcome the challenges and live a happy and healthy life.
Multiple studies utilising functional MRI scans have demonstrated abnormal hyperactivity in specific frontal-subcortical brain circuits in people with OCD. These overactive networks involve interconnected regions like the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia. Excessive activity in these frontal-subcortical loops reflects deficits in cognitive control and behavioural inhibition.
People with OCD appear to have impairment in brain systems that typically allow healthy individuals to suppress intrusive thoughts and resist urges. This neurological dysfunction could explain the inability to disregard obsessive thoughts or stop compulsive behaviours.
Structural MRI studies have also shown reduced grey matter volume in similar frontal-subcortical areas in OCD patients. Thinning of the cortical grey matter implies these brain regions are structurally altered. Changes in the orbitofrontal cortex, anterior cingulate, and basal ganglia likely disrupt emotional processing and impulse control. Alterations in this emotion and impulse regulation circuitry may ultimately drive the obsession and compulsion cycle that devastates the lives of those with OCD.
While the specific causes of these brain changes remain unclear, they likely arise from some combination of genetic factors and environmental influences throughout development.
Uncovering the roots of these neurological abnormalities will enable better targeting of treatments to correct problematic thought patterns at their source. In the meantime, compassion and understanding for those facing the daily battle of OCD is perhaps the most potent medicine of all.
Note: The difference in spelling is simply a matter of regional preference, with "gray matter" being more commonly used in American English and "grey matter" being more commonly used in British English. The term refers to the areas of the central nervous system that primarily consist of neuronal cell bodies, dendrites, and unmyelinated axons, giving these areas a greyish appearance.
Neurotransmitter Abnormalities in OCD
Imbalances in essential neurotransmitters like serotonin have long been implicated in OCD. The effectiveness of selective serotonin reuptake inhibitor (SSRI) medications led researchers to more closely investigate serotonin signalling abnormalities in OCD patients.
Researchers discovered a neurochemical imbalance in the brains of patients with Obsessive-Compulsive Disorder (OCD). Using magnetic resonance spectroscopy, they found a disrupted balance between neurotransmitters glutamate and GABA in two specific regions of the frontal lobes.
The imbalance was linked to both the severity of OCD symptoms and tendencies towards habitual behaviour.
Glutamate is an “excitatory” neurochemical: it facilitates electrical impulses that fire neurons to send information around brain networks. GABA is an “inhibitory” neurotransmitter that works in opposition to glutamate by dampening neural excitability, creating a balance.
PET scans have revealed reduced serotonin transporter binding throughout the brains of those with OCD compared to healthy controls. Lower serotonin transporter levels likely contribute to excessive serotonin activity in the synaptic cleft, which could drive obsessive thoughts and anxieties.
Dopamine - critical for motor control and reward-motivated behaviour - also demonstrates abnormalities in OCD. The basal ganglia, home to dopaminergic neurons, show altered structure and function in imaging studies. Dopamine dysregulation may relate to the repetitive, reward-driven nature of certain OCD compulsions.
Furthermore, dopamine-blocking antipsychotic medications can augment SSRI efficacy for OCD. This synergy implies correcting multiple neurotransmitter imbalances is optimal. While the neurochemistry remains complex, addressing these chemical signalling disturbances with medications alongside behavioural therapy gives hope for recovery.
Pure O form of OCD
Traditionally, obsessive-compulsive disorder is classically considered a disorder of both obsessions and compulsions, some individuals experience only obsessional OCD, nicknamed Pure O. Rather than exhibiting behavioural compulsions, those with Pure O rely primarily on invisible or covert mental rituals to counteract their anxiety-provoking intrusive thoughts.
Pure O often manifests as distressing sexual, violent, or profane obsessions. Without overt compulsions, Pure O frequently goes unrecognised. Raising awareness of this lesser-known form of OCD is critical to ensuring proper diagnosis and treatment.
There is scientific disagreement regarding the possibility of having obsessions without compulsions, commonly referred to as "purely obsessional" or "Pure O." and 5th Edition (DSM-5) — recognises a diagnosis if either obsessions or compulsions are present.
People with excessive health concerns are often included in this category in a few ways. Examples include concerns about mental health problems like cognitive decline, worries about going crazy, or even fears of committing suicide. While such individuals might sound purely obsessional, they are in fact doing compulsions, but these are just not very visible. Covert compulsions are still compulsions, with their need to drive away intrusive thoughts.
However, thought suppression attempts paradoxically lead to increased anxiety and perpetuation of symptoms. In other words, the more one reacts to their unwanted thoughts and distressing feelings, the more meaningful those thoughts and feelings become, also referred to as the OCD cycle, thereby hindering their recovery.

George Ezra the 27-year-old singer-songwriter, who rose to fame in 2014, told how he had been locked in a constant battle with distressing and intrusive thoughts due to a form of obsessive compulsive disorder, known as “Pure O”.
He described how he would compulsively think of the “worst thing”(offensive) to say in any given situation, then punish himself for being a “horrible” person.
Moral Scrupulosity Form of OCD

There are four major subtypes of OCD: contamination, doubt/harm, symmetry/arranging, and unacceptable/taboo thoughts. A subset of individuals with OCD suffers from debilitating moral scrupulosity centred on an excessive fear of sinning or behaving immorally, and it can actually creep in to nearly every kind of OCD.
The term “scrupulosity” is often used to describe religious obsessions, rather concerning an individual moral integrity, and whether one is a good or bad person.
This manifests as obsessions about accidentally committing minor sins or transgressions, and compulsions aimed at gaining moral certainty.
Those with moral scrupulosity OCD may compulsively pray, seek reassurance from others, or mentally review past behaviours to alleviate their anxiety when faced with intrusive thoughts of acting immorally.
Recognising this OCD variant from a religious obsession can enable effective behavioural therapies.
Paedophilia OCD (pOCD)
Paedophilia OCD, also known as POCD, is a type of obsessive-compulsive disorder (OCD) is not the best label to use with its connotation and ambiguity but rather a term that describes the themes that some people with OCD experience and characterised by intrusive fears of being attracted to children and repetitive compulsions aimed at alleviating those fears or doubts and anxiety over the possibility of having such an attraction about being or becoming a paedophile.
It is important to note that having these thoughts does not mean that a person actually has paedophilic tendencies or desires, and distinct from a paedophilic disorder who have sexual fantasies, sexual urges, or non-consensual sexual encounters with children.
Individuals with paedophilia OCD, on the other hand, are not attracted to children; due to their deep-seated fears of attraction, they often avoid children altogether. Therefore, individuals with POCD an official diagnosis often experience extreme distress, guilt, and shame due to their intrusive thoughts involving children.
These thoughts can be highly distressing, unwanted, and go against their true character and values. However, it is crucial to remember that people with POCD are not actually paedophiles, as their distress is a result of their OCD symptoms and not genuine desires or intentions.
The exact causes of POCD are not known, but it is believed to be related to a combination of genetic, neurobiological, and environmental factors. Like other types of OCD, POCD can be managed and treated through various therapeutic approaches.
Cognitive- behavioural therapy (CBT), particularly exposure and response prevention (ERP), is often recommended as a first-line treatment. This therapy involves gradually facing the feared thoughts and situations related to paedophilia, while refraining from engaging in compulsive behaviours.
Perinatal obsessive-compulsive disorder
Maternal OCD, also known as perinatal obsessive-compulsive disorder, is a specific form of obsessive-compulsive disorder that occurs during pregnancy and the post-partum period. It is characterized by intrusive and persistent thoughts or obsessions that are often related to the baby's safety, hygiene, or well-being. These thoughts can be distressing and are usually accompanied by extreme anxiety.
The child’s physician may be the first professional to learn of the infant- and child-rearing difficulties of a distressed mother.
There has been limited research on OCD during and after pregnancy. Recent studies indicate that OCD is more prevalent during this period compared to other times in their life. It is possible for individuals to develop OCD for the first time during pregnancy or after giving birth, while others may experience worsening of pre-existing symptoms.
Whereas, Fairbrother and Abramowitz 2007 proposed that the perinatal period lowers the threshold for OCD development/exacerbation by bringing with it a sudden increase in responsibility for a vulnerable and highly cherished infant.
Mothers with maternal OCD may experience various compulsions or repetitive behaviours aimed at reducing their anxiety or preventing harm to their baby. These compulsions can include excessive cleaning, checking on the baby constantly, seeking reassurance, or avoiding certain situations or objects associated with the obsession.
The exact cause of maternal OCD is not fully understood, but it is believed to be a combination of biological, psychological, and hormonal factors. Hormonal changes during pregnancy and the post-partum period, along with genetic predisposition and pre-existing anxiety or OCD tendencies, can contribute to the development of maternal OCD.
It is also noteworthy, that a mother with a paedophilia OCD may be extremely fearful that she is attracted to her newborn son, so she refuses to change his nappies, feed him, or even spend time alone with him because OCD often preys on what people value most.
Some individuals become distressed and take measures to manage their anxiety or prevent their fears from becoming reality. These measures can include compulsive behaviours like cleaning, praying, rumination, avoiding activities, or even avoiding spending time with the baby, depending on the specific worries.
It is essential for mothers experiencing maternal OCD to seek help and support from healthcare professionals. Treatment options can include therapy, such as cognitive-behavioural therapy (CBT), medication, or a combination of both. Support groups and educational resources can also be beneficial in managing the symptoms and providing guidance for coping strategies.
Religious obsessions in Obsessive-Compulsive Disorder (OCD)

The exact cause of religious obsessions in OCD is not fully understood. However, research suggests that they may stem from a combination of genetic, biological, and environmental factors. People with OCD often have a heightened sense of responsibility and a strong inclination to avoid any perceived harm or wrongdoing. This preoccupation with maintaining moral purity and fear of committing religious sins can manifest as religious obsessions.
In the case of religious obsessions, compulsions may involve excessive praying, confessing sins repeatedly, seeking reassurance from religious figures or texts, or engaging in rituals to combat religious doubts or fears.
It is important to note that having religious thoughts or doubts does not necessarily indicate OCD. OCD is diagnosed when these thoughts become intrusive, distressing, and interfere significantly with daily functioning.
Treatment for religious obsessions in OCD usually involves a combination of Cognitive- behavioural therapy (CBT) and medication, such as selective serotonin reuptake inhibitors (SSRIs), to reduce the frequency and intensity of obsessions and compulsions.
Sexual orientation obsessions in OCD
People with sexual orientation obsessions often experience persistent and intrusive thoughts questioning their sexual identity. They may constantly analyse their own thoughts, feelings, and behaviours, seeking certainty about their sexual orientation. This preoccupation can cause intense anxiety, fear, shame, and distress.
It is important to note that sexual orientation obsessions in OCD do not indicate a person's actual sexual orientation. Individuals experiencing these obsessions may be straight, gay, bisexual, or any other sexual orientation, but their OCD distorts their perceptions and doubts their authentic identity.
The exact cause of OCD is not fully understood, but it is believed to involve a combination of genetic, neurological, and environmental factors. In the case of sexual orientation obsessions, societal stigma, internalized homophobia, or anxiety about non-heteronormative thoughts can contribute to the development or intensification of these obsessions.
Treatment for sexual orientation obsessions in OCD typically incorporates cognitive-behavioural therapy (CBT) and exposure and response prevention (ERP). CBT helps individuals recognise and challenges the irrational thoughts and beliefs associated with their obsessions.
ERP gradually exposes individuals to anxiety-provoking situations or thoughts related to their sexual orientation, while refraining from engaging in compulsive behaviours or seeking reassurance.
Misconceptions about OCD
The term “obsessive-compulsive” is often used loosely to describe people who are meticulous, perfectionist, or preoccupied with order. However, genuine OCD is not indicated by these traits. People with OCD have little control over their intrusive thoughts and often find the obsessions irrational or nonsensical. They gain no pleasure from performing compulsions, only temporary relief from anxiety.
OCD is also not synonymous with phobias like germophobia. Other related terms include contamination OCD, which involves a fear of germs, dirt, or viruses, and harm OCD, which involves a fear of causing harm to oneself or others.
While contamination fears are common in OCD, true phobias cause anxiety about specific objects or situations. OCD obsessions tend to be more general and wide-ranging. Furthermore, phobic avoidance differs from compulsive rituals, which aim to relieve anxiety triggered by obsessions.
OCD is not a colloquial term for tidiness, it is a bit like someone announcing they have a touch of heart disease every time they had indigestion.
Understanding the nuances between OCD and related conditions is vital to combating misconceptions.
Proper education enables more accurate diagnoses and access to treatments explicitly tailored for OCD, which combines medication, psychotherapy, and self-care strategies. With compassionate support, those with OCD can overcome this challenging yet treatable disorder.

Comparing OCD with Other Disorders
Obsessive-compulsive disorder (OCD) is often misunderstood and confused with other conditions. While similarities exist, critical differences separate OCD from disorders like obsessive-compulsive personality disorder (OCPD), perfectionism, and phobias. Recognising the distinct features of OCD is essential to correctly diagnosing and treating this complex condition.
Perfectionism refers to the tendency of individuals to have excessively high standards and expectations for themselves, accompanied by a desire to achieve flawlessness in their work, performance, or appearance. People with perfectionists traits may feel intense pressure to meet these high standards and can be overly critical of their own mistakes or perceived shortcomings, but, OCD is not a character trait.
Phobias, on the other hand, are intense and irrational fears of specific objects, situations, or activities. These fears can be so extreme that they interfere with daily life and cause significant distress. Common phobias include fear of heights, spiders, flying, or enclosed spaces. In the context of Obsessive-Compulsive Disorder (OCD), phobias can manifest as obsessive thoughts and compulsive behaviours related to avoiding the feared object or situation.
For example: Emetophobia
Emetophobia is the fear of vomiting or seeing others vomit. It is a specific phobia that can cause intense anxiety and distress for individuals who experience it. Emetophobia can develop due to various factors, including traumatic experiences related to vomiting or witnessing others vomit, as well as a predisposition to anxiety or specific phobias.
Individuals with emetophobia may have a fear of losing control over their body, fear of being sick in public or social situations, and fear of experiencing nausea or gastrointestinal discomfort.
This phobia can significantly impact their daily lives, causing them to avoid certain foods, situations, or activities that they associate with vomiting.
Cognitive-behavioural therapy (CBT) is a common treatment approach for emetophobia. It focuses on challenging and modifying irrational thoughts and beliefs related to vomiting, gradually exposing individuals to their fears in a controlled manner, and teaching coping skills to manage anxiety. Medications may also be prescribed in severe cases to help alleviate anxiety symptoms.
It's important to seek professional help if emetophobia significantly affects your quality of life. Therapists and medical professionals can provide appropriate guidance and support to manage and overcome this specific phobia.
In the case of OCD, perfectionism can play a role in the development and maintenance of the disorder. Individuals with OCD may feel a need to engage in compulsive behaviours until they reach a state of perceived perfection or until their anxiety reduces.
This can create a cycle where the individual feels driven to repeat these behaviours repeatedly and excessively, leading to significant impairment in their daily life functioning. Ultimately, OCD involves a complex interplay of obsessive thoughts, compulsive behaviours, and the underlying perfectionist tendencies and phobias.
In the case of excessive cleaning or handwashing, individuals with OCD may have an irrational fear of germs or contamination and feel compelled to engage in excessive cleaning or handwashing rituals to alleviate their anxiety.
These rituals provide temporary relief, but the need to repeat them often becomes overwhelming and interferes with daily functioning. It is important to note that excessive cleaning or handwashing may also be influenced by other factors such as anxiety disorders or certain phobias.
Hypochondriasis
Hypochondriasis, also known as illness anxiety disorder, is characterized by an excessive and persistent fear of having a serious medical condition, despite minimal or no evidence of any such condition. Individuals with hypochondriasis often interpret normal bodily sensations as signs of serious illness, leading to heightened concern and excessive doctor visits.
Study by Kellner et al, which showed that patients with high levels of disease fear tended to be more anxious or phobic.
Little comorbidity exists to support the statement that hypochondriasis is an obsessive-compulsive spectrum disorder. Although, patients exist whose hypochondriac concerns are identical in quality to the intrusive thoughts of patients with OCD.
While both hypochondriasis and OCD involve excessive and irrational worry, hypochondriasis is specifically focused on health concerns, while OCD can encompass a wide range of obsessions and compulsions unrelated to health.
However, a closer relationship between hypochondriasis and somatization disorder than between hypochondriasis and OCD.
Hoarding disorder
A hoarding disorder is linked to Obsessive-Compulsive Disorder (OCD) Collecting, arranging, or ordering things.
Hoarding has been classified as a medical disorder for the first time by the World Health Organisation (WHO) in a move that experts say could benefit thousands of people.
Hoarding disorder is characterized by the excessive accumulation and difficulty in parting with possessions, leading to cluttered living spaces and significant distress.
Randomised controlled trials have established cognitive behavioural therapy (CBT) as an effective treatment for hoarding disorder.
During CBT, individuals gradually learn to discard unnecessary items without distress, diminishing their exaggerated perceived need or desire to save these possessions. They also learn to improve their organisation, decision-making, and relaxation skills.
Despite the effectiveness of CBT for a hoarding disorder, a substantial number of hoarding disorder cases remain clinically impaired by their hoarding symptoms after treatment.
Hoarding behaviours often align with the compulsive aspect of OCD, as individuals with hoarding disorder feel compelled to hoard and struggle with intense anxiety when trying to discard items.
While a hoarding disorder can occur independently, it is frequently associated with OCD, as they share similar underlying cognitive and behavioural patterns.
Differences between OCD and OCPD
Obsessive-compulsive personality disorder (OCPD) is a type of personality disorder marked by an overwhelming preoccupation with orderliness, perfectionism, and control. Unlike OCD obsessions, OCPD behaviours are not unwanted - people with OCPD derive pleasure from them.
Men are twice as likely to have OCPD than women. Proximally 1 in 100 people in the United States is estimated to have OCPD.
OCPD behaviours cause no distress and slight impairment.
In contrast, OCD obsessions feel ego-dystonic - they are intrusive, unwanted thoughts that significantly disrupt daily functioning. Those with OCPD adhere rigidly to rules and become upset when others don’t conform. People with OCD have little interest in controlling others.
While OCD and OCPD may appear similar, the inner experience is vastly different. Those with OCD have little control over their anxiety-provoking thoughts. But people with OCPD purposefully organise and check things to their own exacting standards. Recognising this fundamental distinction is critical to proper diagnosis and treatment.
Individuals with OCPD may not show significant impairment until they experience additional disorders, which commonly include obsessive-compulsive disorder (OCD), eating disorders, mood disorders, and alcoholism.
Recognising these distinctions is critical for proper diagnosis and treatment. OCPD and OCD are not the same, even they sometimes overlap. Symptoms that overlap may include paranoia, excessive caution, inability to compromise on set rules or routines, perfectionism and the inability to trust others.
Disorders related to OCD:
Disorders related to OCD are a topic of interest, and they involve various conditions that are linked to obsessive-compulsive disorder. These disorders can have a significant impact on individuals' lives and require attention. Research and understanding in this area are important for the development of effective treatments and support for those affected.
The following are common characteristics among Obsessive Compulsive Related Disorders (also known as OC Related Disorders or OC Spectrum Disorders). However, it is important to note that these disorders can also be differentiated in significant ways.
Body dysmorphic disorder (BDD)
Body dysmorphic disorder (BDD) is a mental health disorder characterised by a preoccupation with perceived flaws or defects in one's appearance that are not observable or are very minor to others. Individuals with BDD often experience significant distress and impairment in their daily lives due to their intense concerns about their physical appearance.
People with BDD may excessively focus on a specific body part or multiple parts, which they believe to be flawed. These perceived flaws can range from imagined or exaggerated to minimal imperfections. Common areas of concern include the skin, facial features, hair, weight, or body shape.
The exact cause of BDD is not fully understood.
However, it is believed to be influenced by a combination of genetic, neurobiological, and environmental factors. Some individuals may have a genetic predisposition to developing BDD, while others may experience triggers such as traumatic events, childhood experiences, or societal pressures related to body image.
Individuals with BDD engage in a range of behaviours in response to their concerns, including repeatedly checking their appearance in mirrors, seeking reassurance from others, comparing themselves to others, and excessively grooming or very likely to seek cosmetic surgery. These behaviours are often time-consuming, interfere with daily functioning, and provide only temporary relief from anxiety.
Treatment for BDD typically involves a combination of psychotherapy, medication, and support from healthcare professionals. Cognitive-behavioural therapy (CBT) is often used to help individuals challenge and modify their distorted thoughts and beliefs about their appearance. Selective serotonin reuptake inhibitors (SSRIs), a type of antidepressant medication, may also be prescribed to reduce obsessive thoughts and compulsive behaviours associated with BDD.
It is important for individuals with BDD to seek professional help as early as possible, as the disorder can significantly impact their overall well-being and quality of life. With proper treatment and support, many people with BDD can experience symptom reduction and improved functioning.
Body Focused Repetitive Behaviours (BFRBs)
Body Focused Repetitive Behaviours (BFRBs) is considered a type of self-grooming behaviours that involve repetitive, compulsive actions focused on the body. These behaviours often serve as a way to cope with stress, anxiety, or other emotional or mental health issues. Examples of BFRBs include hair pulling (Trichotillomania), skin picking (Dermatillomania), and nail-biting (Onychophagia).
BFRBs are considered to be a form of impulse control disorder and can be classified as a type of obsessive-compulsive disorder (OCD) or related disorders under a compendium of psychiatric diagnoses. They are often characterised by an irresistible urge or urge-like sensation that drives the person to engage in these behaviours, even if they are aware of the negative consequences.
The exact cause of BFRBs is not fully understood, but it is believed to be a combination of genetic, environmental, and neurobiological factors. BFRBs can be triggered or exacerbated by stress, anxiety, or other emotional triggers, which can lead to a cycle of tension, relief through engaging in the behaviour, and subsequent guilt or shame afterwards.
Treatment for BFRBs often involves a multidisciplinary approach, including therapy, medication, and support groups. Cognitive-behavioural therapy (CBT) is commonly used to help individuals identify and manage triggers, develop coping strategies, and challenge negative thought patterns associated with the behaviours. Medication, such as selective serotonin reuptake inhibitors (SSRIs), may be prescribed in some cases to help manage underlying anxiety or depressive symptoms.
It is important for individuals experiencing BFRBs to seek professional help, as these behaviours can have a significant impact on their daily functioning, self-esteem, and overall well-being. Early intervention and appropriate treatment can help individuals gain control over their behaviours and improve their quality of life.
Olfactory Reference Syndrome (ORS)
Olfactory Reference Syndrome (ORS) is a psychological disorder characterised by an individual's belief that they emit a foul or unpleasant body odour, despite little or no objective evidence of such odour.
People with ORS often experience excessive anxiety and distress about their perceived body odour, leading to significant impairment in their social and occupational functioning.
The exact cause of ORS is not fully understood, but it is believed to be related to underlying psychological factors, such as obsessive-compulsive disorder (OCD) or other anxiety disorders. Individuals with ORS may engage in compulsive behaviours, such as excessive washing or using strong fragrances, in an attempt to mask or eliminate the perceived odour.
However, these behaviours often provide only temporary relief and can exacerbate the condition.
ORS typically manifests in adolescence or early adulthood and tends to be chronic if left untreated. It can cause significant distress and lead to social isolation, impaired relationships, and decreased quality of life.
Treatment for ORS generally involves a combination of psychotherapy, such as cognitive-behavioural therapy (CBT), and medication, such as selective serotonin reuptake inhibitors (SSRIs), to address the underlying psychological factors contributing to the disorder.
Overall, ORS is a complex psychological condition that affects an individual's perception of their own body odour. With appropriate treatment and support, individuals with ORS can learn to manage their symptoms and improve their overall well-being.
Misophonia
People with Misophonia experience intense rage or irritation when they encounter specific trigger sounds, such as chewing, coughing, or tapping. This reaction is thought to be a result of their brain perceiving these sounds as a threat or danger. The exact cause of Misophonia is still not fully understood, but it is believed to involve a combination of genetic, neurological, and psychological factors.
On the other hand, people with Obsessive-Compulsive Disorder (OCD) have recurring, intrusive thoughts, ideas or images (obsessions) that cause anxiety, and they often try to alleviate this anxiety through repetitive behaviours or rituals (compulsions).
While Misophonia primarily affects the way individuals respond to specific sounds,
OCD is a broader condition that can manifest in various forms, including obsessive thoughts unrelated to triggers or sounds.
Both conditions can significantly impact an individual's daily life and cause distress. It is important for people with Misophonia or OCD to seek professional help for proper diagnosis and management of symptoms. Treatment options may include therapy, medication, or a combination of both, depending on the severity of the condition.
Paediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections (PANDAS)
In 1998, Dr. Susan Swedo identified a subtype of OCD in children, which she referred to as PANDAS, stands for Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections.
It is a rare condition that is believed to be triggered by a streptococcal (strep) infection, particularly a strep throat. PANDAS is characterized by sudden and dramatic onset of obsessive-compulsive disorder (OCD) symptoms, as well as other neurological and behavioural changes in children.
In PANDAS, the immune system mistakenly attacks healthy cells in the brain, leading to inflammation and dysfunction. This immune response is thought to be triggered by antibodies produced in response to the strep infection. The exact mechanism of how this autoimmune response occurs is not fully understood.
The symptoms of PANDAS can include severe anxiety, intense and irrational fears (phobias), tics, mood swings, difficulty concentrating, irritability, and deterioration in academic performance. These symptoms can appear suddenly or worsen rapidly, often following a strep infection, and the symptoms of OCD or tic symptoms suddenly become worse following a strep infection.
Diagnosis of PANDAS involves a thorough evaluation of the child's symptoms, medical history, and laboratory tests to identify any evidence of a recent or ongoing strep infection. Typically, first appears in childhood from age 3 to puberty. Treatment usually involves the use of antibiotics to treat the underlying strep infection and anti-inflammatory medications to reduce brain inflammation. In some cases, other treatments such as cognitive-behavioural therapy or immunomodulatory therapies may be recommended.
It is important to note that PANDAS is still a topic of ongoing research, and there may be differing opinions and approaches to its diagnosis and treatment within the medical community.
Orthorexia nervosa
Orthorexia nervosa (ON) is a condition described as a pathological obsession with healthy eating. It has been linked to body dissatisfaction, alcohol, and drug use. There is an overlap with those of eating disorders like anorexia nervosa and bulimia nervosa.
Disorders Confused with OCD:
There are disorders that can be mistaken for OCD. It's important to note the differences to ensure accurate diagnosis and treatment.
These disorders show some common characteristics and overlapping features, but can also be distinguished from OCD and one another by a well-trained mental health provider.
Tourette Syndrome
Tourette Syndrome is a neurological disorder that is characterized by repetitive, involuntary movements and vocalizations known as tics. These tics can range from mild to severe and may vary in frequency and intensity over time.
The exact cause of Tourette Syndrome is not fully understood, but it is believed to involve a combination of genetic and environmental factors. It is thought to be a result of abnormalities in the brain involving the movement and communication pathways.
The abnormal movements and vocalizations exhibited in Tourette Syndrome are caused by disruptions in the normal regulation of neurotransmitters, which are the chemical messengers in the brain. Specifically, an imbalance in dopamine and serotonin levels in the brain is believed to play a role in the development of tics.
Tourette Syndrome often begins in childhood, typically between the ages of 2 and 15. The severity of the condition can vary widely among individuals. Some people may experience mild tics that do not significantly impact their daily lives, while others may have more severe tics that interfere with their ability to function and may require treatment.
Treatment for Tourette Syndrome focuses on managing the symptoms and improving quality of life. This can include medications, behavioural therapy, and support groups. While there is no cure for Tourette Syndrome, many individuals with the condition are able to lead fulfilling and productive lives with appropriate management and support.
Impulse control disorders
Impulse control disorders are a group of mental health conditions characterized by a failure to resist impulses or urges that may be harmful or detrimental to oneself or others. These disorders involve a disruption in the brain's ability to regulate emotions and control behaviours.
There are several types of impulse control disorders, including kleptomania (an irresistible urge to steal), pyromania (an uncontrollable urge to set fires), intermittent explosive disorder (recurrent episodes of impulsive aggressive behaviour), and compulsive gambling (an inability to resist the urge to gamble).
The exact cause of impulse control disorders is not fully understood.
However, it is believed that a combination of genetic, environmental, and neurobiological factors can contribute to their development. Some individuals may have a genetic predisposition to impulsivity, while others may have experienced traumatic events or have difficulties in regulating their emotions.
Treatment for impulse control disorders typically involves a combination of medication, psychotherapy, and support groups. Medications, such as selective serotonin reuptake inhibitors (SSRIs) or mood stabilizers, may be prescribed to help regulate emotions and reduce impulsive behaviours. Psychotherapy, such as cognitive-behavioural therapy (CBT), can help individuals develop coping strategies, improve self-control, and address any underlying psychological issues.
It is important for individuals with impulse control disorders to seek professional help, as these conditions can significantly impact their lives and relationships. With proper treatment and support, individuals can learn to manage their impulses and regain control over their behaviours.
Autism Spectrum Disorders (ASD)
In some cases, individuals with ASD may also exhibit OCD tendencies or behaviours. These can manifest as repetitive rituals, extreme preoccupation with certain objects or thoughts, and a need for strict routines. However, it is important to note that not all individuals with ASD will also have OCD tendencies, and vice versa.
- “Stereotyped” behaviours like following rigid routines, an “obsessive” interest in something
- Usually have thoughts and behaviours that only focus on repeating things.
- Don’t try to prevent their thoughts.
- Have severe problems with social interactions
The co-occurrence of ASD and OCD tendencies can present additional challenges for individuals. These individuals may experience difficulties in managing their obsessions and compulsions, which can significantly impact their daily functioning and quality of life.
Psychotic disorders
Psychotic disorders are a group of mental illnesses characterized by abnormal thinking and perceptions. They can include symptoms such as hallucinations, delusions, disorganized thinking, and unpredictable behaviour. These disorders can significantly impact a person's thoughts, emotions, and behaviour, leading to difficulties in functioning in daily life.
Individuals with Psychotic Disorders/Schizophrenia and people with OCD both may have:
- Strange or bizarre thoughts. Thoughts that include sexual violent or religious themes
- Have delusions.
Their thoughts aren’t based in reality, but the person believes the thoughts to be true.
It is important to note that psychotic disorders and OCD are distinct conditions, but they can occasionally coexist or share certain symptoms.
The exact cause of these disorders is still not fully understood, but it is believed to result from a combination of genetic, biological, and environmental factors.
Treatment for psychotic disorders often involves a combination of medication, such as antipsychotics, and psychotherapy.
For OCD, cognitive-behavioural therapy (CBT) and medications like selective serotonin reuptake inhibitors (SSRIs) are commonly used.
Conclusion
Obsessive-compulsive disorder (OCD) is a complex psychiatric condition that can significantly disrupt the lives of those it afflicts. As highlighted throughout this article, OCD is characterised by intrusive, irrational thoughts and anxiety-driven compulsive rituals that trap sufferers in a relentless cycle of obsessions and compulsions. While OCD certainly poses challenges, knowledge and compassion are powerful tools for confronting this condition.
From a prevalence of 2-3% to striking in early adulthood, key statistics provide a snapshot of OCD’s impact on the population. We traced the evolution of OCD’s conceptualisation from early psychoanalytic theories to modern neurobiological understandings. Brain imaging studies reveal abnormalities in frontal-subcortical circuits that drive rigid thoughts and behaviours. New treatment modalities like CBT with mindfulness offer hope. While genetic vulnerabilities exist, environmental influences and empowered self-care can help overcome OCD.
The future is bright for those with OCD. Though sometimes debilitating, symptoms need not define one’s entire life narrative. With compassionate understanding and evidence-based treatment, OCD’s grip can be broken. Periods of remission are possible. We all have a role to play in fostering acceptance for those dealing with mental health challenges.
There are usually other problems such as depression, anxiety, autistic spectrum disorder or an eating disorder like Orthorexia Nervosa, associated with a pathological obsession with healthy eating, poor body image, or a preoccupation with their personal appearance.
Our shared humanity calls us to choose understanding over judgment patience over frustration. Progress comes one small step at a time.
It is important for individuals with Obsessive-compulsive disorder to seek professional help from qualified mental health professionals who specialise in OCD or anxiety disorders. They can provide appropriate diagnosis, support, and guidance for managing and treating symptoms. Thus, the information supplied should not be used as a substitute for any qualified medical advice.