- in Mental Health by Tony
Understanding Agnosia: Exploring the Complexities of Perception Impairment.
In the world of neuroscience and psychology, there are intriguing conditions that challenge our fundamental understanding of perception.
One such condition is agnosia, which disrupts somebody’s ability to recognise or interpret sensory information. Agnosia usually affects only a single information pathway in the brain. If you have this condition, you can still think, speak, and interact with the world.
While it may sound like a relatively simple concept, delving into the complexities of agnosia reveals a rich tapestry of mental processes and brain functions at work. In this article, we explore agnosia, unravelling its various forms and shedding light on what it truly means to grapple with this mysterious disorder.
Join us as we dig deeper into understanding how perception impairment can manifest in fascinating and perplexing ways.
More...
Agnosia (in Greek gnosis- "not knowing") is a neurological condition in which a patient is unable to recognise and identify objects, persons, or sounds using one or more of their senses in spite of their normally functioning senses.
Therefore, agnosia is a neurological disorder that affects a person’s ability to recognise and interpret sensory information. It can occur in various forms, each involving a different sensory modality.
There are three main types of agnosia: visual, auditory, and tactile.
Let’s commence with a short summary of the different spectrums of agnosia:
1. Visual Agnosia: This is the most common form of agnosia and affects a person’s ability to recognise visually presented objects, faces, or shapes. They may still have intact vision, but their brain cannot correctly process and interpret visual information.
2. Auditory Agnosia: This type of agnosia impacts a person’s ability to recognise and interpret sounds, such as speech or environmental noises. They may hear sounds, but have difficulty understanding their meaning or distinguishing between those sounds.
3. Tactile Agnosia: This form of agnosia affects a person’s sense of touch, making it challenging for them to recognise objects through touch alone. They may need help identifying shapes, textures, or temperatures through contact.
4. Prosopagnosia: Also known as face blindness, prosopagnosia is a specific type of visual agnosia where individuals cannot recognise familiar faces, including those of family members or close friends. They may rely on other cues, such as voice or clothing, to identify people.
5. Anosognosia: Anosognosia refers to a lack of awareness or recognition of one’s own illness or disability. This can occur in various neurological conditions, including agnosia itself. Individuals with anosognosia may deny or be unaware of their impairment, making it challenging to seek treatment or support.

It is important to note that agnosia can occur due to brain injuries, or degenerative neurological conditions, and can vary in severity. But stroke, is the most common cause of aphasia. Treatment options may include rehabilitation therapy, adaptive strategies, and support from healthcare professionals.
Let’s now look at each situation in more detail.
Visual Agnosia: Unravelling the Mystery of Impaired Object Recognition

Visual agnosia is a fascinating disorder that hinders an individual’s ability to recognise and identify objects they see. How our brain processes visual information helps us, from learning as children, to how we see the world and interact with our environments throughout our lives.
Because of the ease with which we rely on these perceptual processes, we tend to overlook the complexity behind visual information processing. It is not related to any issues with vision or intelligence, but rather arises from a disruption in higher-level of visual processing we once took for granted.
Visual agnosia is a condition where you can’t name or describe the purpose of an object just by looking at it. However, you can still physically reach for and pick up the object. Once you have it in your hands, you can use your sense of touch to identify what it is or how it’s used.
People with visual agnosia may still have perfectly functional eyes and can detect shapes, colours, and other essential visual features; however, they struggle to make sense of these elements as meaningful objects.
This perplexing condition often leaves those affected unable to identify everyday items, such as a pen or a cup, despite having encountered them countless times before. Even familiar faces become unrecognisable, causing difficulties in their interpersonal relationships.
As scientists delve into the complexities of perception impairment, they encounter challenges in unravelling the precise mechanisms underlying this puzzling disorder. Despite these challenges, ongoing research is shedding light on understanding visual agnosia and providing hope for potential treatments or interventions in the future.
Auditory Agnosia: Decoding the Challenges of Processing Sounds

In the late nineteenth century, Freud first used the term agnosia to describe a selective auditory recognition deficit as distinct from a primary disturbance in language faculties.
Agnosia is like listening to a foreign language without understanding any of the words. Even though the sounds may be familiar, their meaning still needs to be discovered, making communication incredibly difficult.
Auditory agnosia is a complex condition that affects an individual’s ability to recognise and interpret sounds. Those with auditory agnosia cannot identify ordinary sounds like phone ringing or birds chirping. This impairment stems from damage to specific brain areas responsible for processing auditory information.
Individuals with auditory agnosia often struggle in everyday situations that rely on sound recognition, such as understanding speech or following conversations. They may find it difficult to distinguish between similar sounds, leading to confusion and frustration.
Despite having normal hearing abilities, people with this form of agnosia cannot understand what they hear. Research suggests that individuals with auditory agnosia have intact basic hearing abilities but fail to extract meaningful information from sound stimuli due to disruptions within their brain pathways.
By unravelling the complexities associated with this disorder, researchers hope to develop effective interventions and assistive technologies for those affected by auditory agnosias.
Tactile Agnosia: Understanding the Complexities of Touch Perception

Child in therapy sensory stimulating room, snoezelen. Child interacting with colored lights bubble tube lamp during therapy session.
The Tactile Sense
Our tactile sense keeps us in touch with our environment. Our sense of touch is derived from a range of receptors in our skin that take messages about pressure, vibration, texture, temperature, pain and the position of our limbs and pass it through our nervous system to the brain. Our tactile receptors fall into four groups.
1. Mechanoreceptors: These receptors pick up sensations like pressure, vibration and texture.
2. Thermoreceptors: These receptors pick up sensations of hot and cold.
3. Pain receptors (nociceptors): For noxious stimuli, and we have over 3,000,000, and they are found in the skin, bones, some organs, blood vessels and muscles. A physiological process by which body tissues are protected from damage.
4. Proprioceptors: These receptors provide feedback to the brain on the position of different parts of the body in relationship to each other. Located in tendons, joint capsules and muscles.
This is why people with tactile agnosia may have difficulty identifying familiar objects by touch alone, such as a key or a coin.
They often rely on visual cues to compensate for their impaired sense of touch, which can be challenging when vision is limited.
Tactile agnosia can also affect an individual’s perception of different textures and temperatures. Someone with tactile agnosia may not be able to discern between a rough surface and a smooth one when using their hands only.
Tactile agnosia is a condition that affects an individual’s ability to recognise objects through touch. It is caused by damage or dysfunction in the brain regions responsible for processing sensory information from the skin.
Understanding the tactile sense enables us to appreciate how finely balanced this system is. A sensory processing disorder that affects the sense of touch can significantly impact upon a person’s life.
Tactile agnosia requires insight into the complex process of touch perception and how it can be disrupted. Although this impairment can present challenges and frustrations for individuals affected, advancements in research and therapy offer hope for a better understanding and management of this condition.
Overall, these types of agnosias highlight how complex perception impairments can be, while showcasing how different senses play critical roles in our ability to understand and interact with the world around us.
There are two forms of agnosia based on causes - Apperceptive and Associative:
1. Associative agnosia: It is a failure in recognition despite no deficit in perception. Associative agnosia patients can typically draw, match or copy objects but couldn't recognise the item, while apperceptive agnosia patients cannot.
2. Apperceptive agnosia: It is a failure in recognition due to deficits in the early stages of perceptual processing.
Associative Visual Agnosia: Exploring the Disrupted Connections between Perception and Memory

Associative agnosia is a specific type of agnosia that affects the ability to recognise and identify objects, even though primary visual perception remains intact.
Individuals with associative visual agnosia may be able to see an object clearly but struggle to understand its meaning or purpose. This impairment arises from disrupted connections between perception and memory, making it difficult for individuals to relate what they see, regardless of their prior knowledge or experiences.
Patient CK's copy of a geometric configuration. The numbers assigned to his copy indicate the order in which the lines were drawn and show that he copies in a very literal fashion, failing to integrate lines 1, 2, 8, and 9 into a single shape.
Patient CK, an individual with associative agnosia, was reasonably good, although the process by which he copied indicates a failure to bind the contours into a meaningful whole shape.
One of the important claims of associative agnosia is that perception is intact, and it is meaning that is inaccessible.
Symptoms of Associative Agnosia
- Difficulties were recognising familiar people, objects, or places.
- Inability to identify everyday items by sight alone.
- Challenges understanding the function or use of things.
- Sometimes accompanied by other deficits in language processing.
Causes of Associative Agnosia
- Brain damage in areas responsible for connecting perception and memory, such as the temporal lobes.
- Injury or illness affecting neural pathways involved in visual recognition processes.
By studying associative agnosia, researchers hope to gain deeper insights into how perception and memory interact within our brains. Understanding this complex condition can lead to improved diagnostic tools and tailored rehabilitation strategies for those affected by agnosic impairments.
Apperceptive Agnosia: Examining the Breakdown of Visual Processing
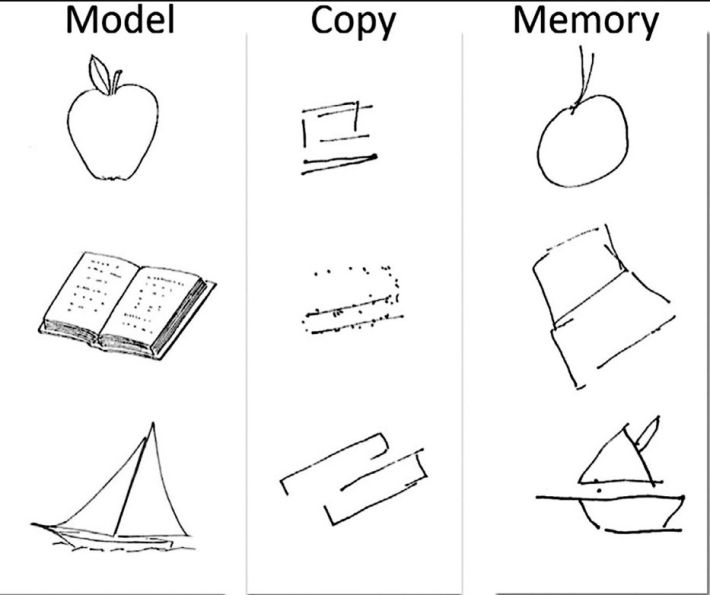
Drawing in copy and from memory performed by DF, a patient with apperceptive agnosia. Figure from Milner AD, Cavina-Pratesi C (2018). Chapter 13—Perceptual deficits of object identification: apperceptive agnosia. In: G Vallar & HB Coslett (Eds.), Handbook of clinical neurology. Elsevier, with permission from Elsevier.
Individuals with apperceptive agnosia, also known as visual form agnosia or object agnosia, are unable to recognise visible objects, even if they can accurately describe their size, texture, and some aspects of their shape. On the other hand, drawing from memory is generally possible, which demonstrates the integrity of the knowledge relating to the visual aspects of the object shown above.
A specific type of agnosia, known as apperceptive agnosia, results in a breakdown of visual processing. Individuals with this condition struggle to recognise and interpret visual stimuli accurately. They may have difficulty perceiving shapes, objects, or even faces.
It is argued that apperceptive object agnosia (generally now known as visual form agnosia) was a misnomer and not an agnosia, but rather a form of “imperception”.
Imperception was coined by Hughlings Jackson (1876), referring to a condition or state of being where one is unable to perceive or consciously recognise certain sensory stimuli or information despite their presence or availability. It pertains to a lack of awareness or understanding of specific sensory inputs or events occurring in the environment, often related to a neurological or cognitive impairments.
Warrington (1985), for example, felt impelled to argue that individuals whose recognition failure is caused by a deficit in elementary shape perception or discrimination could not be considered as having apperceptive agnosia, but only as having pseudoagnosia.
This impairment occurs due to damage or dysfunction in the occipitotemporal region of the brain, where visual information is processed. The disruption prevents the affected person from coherently representing what they see. Lesions are typically bilateral and often caused by carbon monoxide poisoning (Bridge et al., 2013), but can also be vascular, degenerative or traumatic in origin.
Apperceptive agnosia can be diagnosed through cognitive tests assessing a person’s ability to identify or match objects based on appearance. Treatment for this condition typically involves rehabilitation programs to improve perception and object recognition skills.
Prosopagnosia: Investigating the Inability to Recognise Faces (Face blindness)

A specific type of agnosia, known as prosopagnosia, causes individuals to be unable to recognise faces. In 1889, Freund, a German neurologist of Breslau, described a case of visual recognition deficit that he named optic aphasia, and he interpreted as a consequence of the disconnection of visual from language areas.
- People with prosopagnosia may struggle to differentiate between familiar faces and fail to process facial expressions accurately.
- Prosopagnosias use cues such as voice, hairstyle, or clothing to identify people they know.
- This condition can make social interactions challenging and lead to feelings of isolation and frustration.
Published in February 2023 in Cortex, the study findings indicate that as many as one in 33 people (3.08 percent) may meet the criteria for face blindness, or prosopagnosia. This translates to more than 10 million Americans, the research team said.
Studies suggest that prosopagnosia might be caused by abnormalities in the brain’s fusiform face area (FFA), which is responsible for processing facial recognition.
Difficulty with facial recognition can also occur in Alzheimer’s disease. It happens because brain deterioration can damage this region. A new study published on 26 July, 2023 by Neurology suggested that a gene variant may cause an impaired in the sense of smell before any symptoms of Alzheimer’s disease, starts to appear.
Autism may also cause difficulty recognising faces. Children with autism spectrum disorders may learn to recognise faces differently. Parents with children on the spectrum often speak about their kids’ difficulty recognising faces, even those of friends and relatives. They may find it more difficult to understand another person’s identity or emotional state. The results from a recent study (Minio-Paluello et al., 2020) revealed prosopagnosia potentially occurs in more than 36% of autistic adults without intellectual disability.
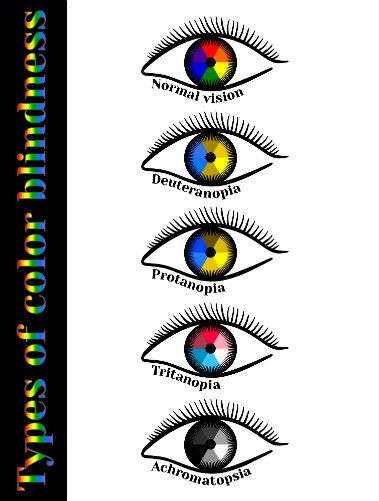
Achromatopsia (colour blindness)
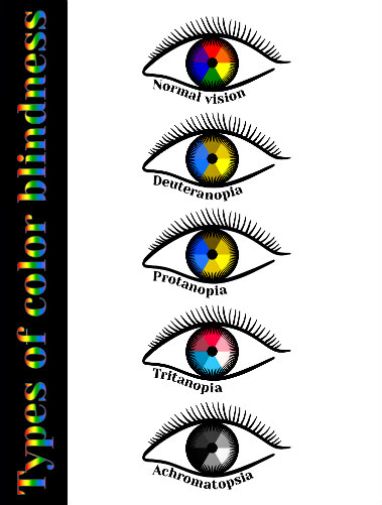
Colour blindness, also known as colour vision deficiency, refers to a condition where an individual has difficulty perceiving certain colours. There are several different types of colour blindness, each with its unique characteristics.
Here are the most common types:
1. Deuteranopia: People with deuteranopia lack the ability to perceive the green colour. Instead, they may see green colours as gray or brown. This type of colour blindness affects around 1% of males.
2. Protanopia: Protanopia refers to the inability to perceive the red colour. Those with protanopia may see reds as brownish or gray. Similar to deuteranopia, protanopia is also more common in males, affecting around 1% of them.
3. Tritanopia: Tritanopia is relatively rare and affects the ability to perceive the blue colour. Individuals with tritanopia may confuse blue colours with green or yellow. It is an inherited condition, but is not gender-specific. Tritanomaly (blue-weak) – Individuals have blue cones and can usually see some shades of blue.
4. Achromatopsia: Achromatopsia, also known as total colour blindness, is a more severe form of colour blindness. People with achromatopsia cannot see any colours and perceive the world in shades of gray (Monochromacy). The rate of achromatopsia is identical in men and women, and this condition is extremely rare, affecting around 1 in 33,000 individuals. ( AchromaCorp.org)
5. Achromasy: Achromasy, also referred to as acquired achromatopsia, occurs due to damage to the optic nerve or other parts of the visual system. People with achromasy may gradually lose their ability to see colours or lose it suddenly due to an injury or illness.
It is important to note that while these are the most common types of colour blindness, there are other variations and degrees of colour vision deficiency.
If you suspect you may have a problem with colour perception, it is recommended to consult with an eye doctor for a proper diagnosis and understanding of your specific condition.
Not all forms of colour blindness are the same. Based on the cause and symptoms, a distinction is made between colour deficiencies, partial colour blindness and total colour blindness.
A person can be born with colour perception deficiencies or develop them over the course of their life. Achromatopsia, which is acquired colour blindness with an inability to identify any colour. A lesion in the left occipitotemporal region can usually cause this.
Not to be confused, Colour blindness, also known as colour vision deficiency, is a condition in which a person has difficulty distinguishing between specific colours, like a red-green colour deficiency.
A genetic defect usually causes it and affects the perception of colours, making it challenging to identify particular shades or differentiate between colours that others can easily see.
Achromatopsia and achromasy are both conditions that affect a person’s ability to see colour, but they have some key differences.
Achromatopsia, or total colour blindness, is a rare genetic condition characterised by the complete absence of colour vision. Those with achromatopsia see the world only in black, white, and shades of grey.
In addition to the lack of colour perception, individuals with achromatopsia often experience other vision problems, such as extreme sensitivity to light and reduced visual acuity.
On the other hand, achromasy is a term used to describe a broader range of colour vision deficiencies. While achromatopsia refers specifically to the absence of colour vision, achromasy can refer to both partial and complete loss of colour perception.
It encompasses conditions such as monochromacy, where individuals are only able to see in shades of grey, as well as other forms of colour vision deficiencies such as dichromacy (seeing only two primary colours) or trichromacy (seeing three primary colours but with altered perception).
In summary, achromatopsia is a specific form of achromasy characterised by the complete absence of colour vision, while achromasy is a broader category that includes various forms of colour vision deficiencies.
Environmental chemicals – Even at low levels, carbon disulphide and lead can cause colour blindness.
Alcohol consumption – Reduced colour discrimination can be a symptom of alcoholism, with blue-yellow being particularly affected.
Olfactory agnosia
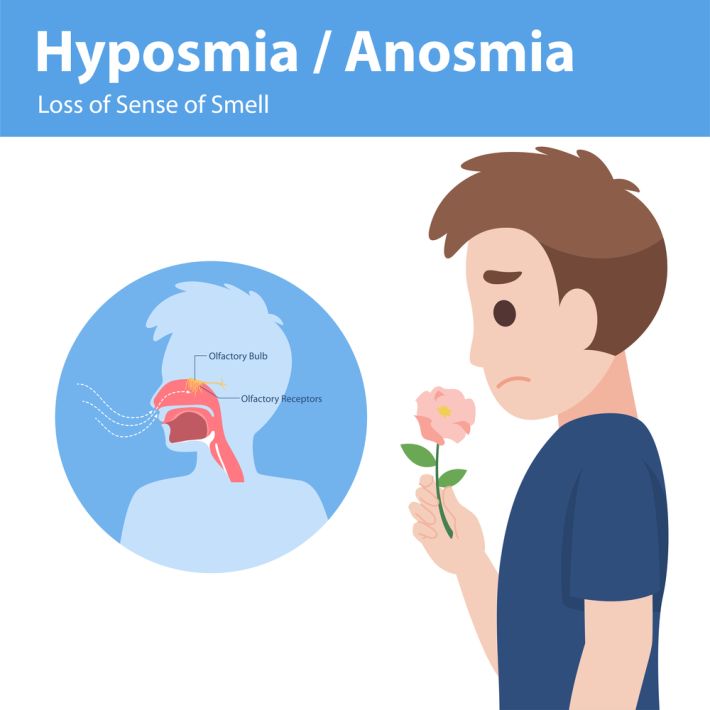
Loss of smell in agnosia can occur as a result of damage to the brain regions responsible for processing and interpreting olfactory information. Agnosia refers to a condition where a person is unable to recognise or interpret sensory information correctly, and this can include olfactory agnosia, or the inability to perceive or identify smells.
There are several potential causes of olfactory agnosia, including brain injuries, strokes, certain neurological disorders, or even the natural ageing process. When the brain regions involved in smell processing are damaged or impaired, it can result in a loss of smell perception.
Treatment for olfactory agnosia will largely depend on the underlying cause and may involve a combination of therapies. In some cases, occupational therapy or sensory retraining exercises can help to improve olfactory function.
Additionally, techniques such as smell training, where a person is exposed to different scents to help retrain their olfactory system, may be utilised.
It's important to consult with a medical professional if you or someone you know is experiencing a loss of smell due to agnosia. They can help determine the underlying cause and recommend appropriate treatment options to manage the condition.
Hyposmia and anosmia are both conditions that result in a loss of smell.
Hyposmia refers to a partial loss of smell, whereas anosmia refers to a complete loss of smell. These conditions can have various causes, including sinus infections, nasal polyps, head injuries, viral infections, and certain medications.
If you are experiencing a loss of smell, it is important to consult with a medical professional to determine the underlying cause and receive appropriate treatment.
In some cases, the loss of smell may be temporary and resolve on its own. However, in cases where the loss of smell is persistent, there are a few strategies that can help manage the condition:
1. Practice good nasal hygiene: Keeping your nasal passages clean and moisturized can help improve your sense of smell. You can do this by using a saline nasal spray or rinsing your nose with a neti pot.
2. Use smell training: Smell training involves exposing yourself to different scents on a daily basis to help improve your sense of smell. This can be done by using essential oils or smelling common household items.
3. Avoid irritants: Certain irritants, such as cigarette smoke or strong chemical odours, can further damage your sense of smell. It is important to avoid exposure to these irritants to help maintain whatever level of smell you have.
4. Stay hydrated: Drinking plenty of water can help keep your nasal passages moist, which can aid in the sense of smell.
5. Seek support: Joining support groups or online communities can provide valuable information and emotional support for individuals with hyposmia and anosmia. It can also be helpful to connect with others who are experiencing similar challenges.
Remember, it is essential to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan. They can provide expert guidance based on your specific condition and needs.
Olfactory agnosia and Anosmia:
Olfactory agnosia and anosmia are both conditions that affect a person's sense of smell, but they differ in their underlying causes and symptoms.
Olfactory agnosia, also known as smell agnosia or specific anosmia, refers to the inability to recognise or identify specific smells, despite having a normal sense of smell.
It is a neurological condition that is often associated with brain damage or injury, such as a stroke or head trauma. People with olfactory agnosia may find it difficult to distinguish between different odours, or may be unable to identify familiar smells. This condition can significantly impact a person's ability to perceive and interpret their environment.
On the other hand, anosmia is a complete loss of the sense of smell. It can be caused by a variety of factors, including nasal congestion, sinus infections, nasal polyps, or neurological conditions such as Parkinson's disease or Alzheimer's disease.
Anosmia can be temporary or permanent, and can range from partial loss of smell to a complete inability to detect any odours. Individuals with anosmia may struggle with everyday activities such as detecting spoiled food, perceiving environmental hazards, or enjoying the pleasurable aspects of taste and smell.
In summary, olfactory agnosia is the inability to recognise specific odours despite a normal sense of smell, whereas anosmia refers to a complete loss of the sense of smell. Olfactory agnosia is often associated with brain damage or injury, while anosmia can have various causes, ranging from nasal obstruction to neurological conditions. Both conditions can have a significant impact on a person's quality of life and should be evaluated by a medical professional.
Living with agnosia:
Living with agnosia can be a challenging experience, as it can disrupt numerous aspects of daily life.
Navigating the Environment:
For someone with agnosia, navigating through spaces can be difficult due to impaired perception of depth and spatial relationships. This means they might bump into furniture or misjudge distances when walking upstairs or crossing roads.
Simple tasks like cooking can also pose risks, since accurately gauging heat levels or handling sharp utensils becomes problematic.
Impaired Facial Recognition:
Recognising familiar faces becomes an arduous task for individuals with impaired facial recognition. They may have trouble identifying family members, close friends, or even themselves in photographs. As a result, social interactions become overwhelming and frustrating, as they cannot easily distinguish between people they know and strangers.
Impaired Senses:
Agnosia affects more than just visual recognition; it also extends to other senses, such as touch, hearing, and smell. Some individuals may not realise they are touching something hot until it causes burns, while others may struggle to decipher ambient noises like sirens signalling danger. (Fire or Gas alarm)
These daily safety concerns make independent living challenging without support from caregivers or assistive devices.
Coping Strategies:
While there is no cure for agnosia at the present time, there are coping strategies that can help individuals manage their condition:
- Routines: Establishing predictable routines helps create familiarity, which aids recognition despite impaired perception.
- Labels: Clearly labelling objects around the house enables easier identification.
- Social Support: Surrounding oneself with supportive family members and friends who understand one’s condition helps reduce feelings of isolation.
- Adaptive Technologies: Utilising technology such as voice-activated assistants or specialised smartphone apps can assist with tasks like object identification or navigation.
- Professional Assistance: Seeking assistance from healthcare professionals, such as occupational therapists or speech-language pathologists, can provide strategies and techniques to cope with everyday challenges.
Comorbidity of Agnosia in health and disease
Agnosia is a complex condition that can coexist with various other health issues. Here are some notable comorbidities:
- Neurological disorders: Agnosia often accompanies conditions like Alzheimer’s disease, Parkinson’s disease, or traumatic brain injury. This suggests that damage to specific brain regions can lead to both agnosia and these neurological disorders.
- Psychiatric disorders: Individuals with schizophrenia or major depressive disorder may also experience symptoms of agnosia. These psychiatric conditions significantly impact perception and cognition, making them susceptible to developing agnosic symptoms.
- Learning disabilities: Some children with learning disabilities, such as dyslexia or ADHD, may exhibit signs of agnosia. Difficulties in understanding objects or recognising faces could be related to the underlying perceptual impairments associated with their primary learning disability.
Understanding these comorbidities helps healthcare professionals develop more comprehensive treatment plans for those affected by agnosia. By addressing all aspects of a patient’s diagnosis, a better quality of life can be achieved through tailored interventions and support systems.
Agnosia in Mental Health
Agnosia is a rare condition that affects an individual’s ability to recognise and interpret sensory information correctly.
It can occur due to damage to specific brain areas, impairing perception and understanding of the world. In mental health, agnosia is often seen in individuals with neurological disorders such as Alzheimer’s disease or schizophrenia.
Effects on Perception
People with agnosia may struggle to identify objects or understand their purpose, even if their senses are intact.
For example, they may not be able to recognise familiar faces or accurately name everyday things like keys or a pen. This impairment can significantly impact daily life activities and communication with others.
Challenges in Diagnosis
Diagnosing agnosia in mental health can be challenging due to its overlap with other cognitive disorders and symptoms commonly associated with psychiatric conditions.
The complex nature of perception impairment requires careful assessment by healthcare professionals experienced in both neurology and mental health fields.
An accurate diagnosis is crucial for implementing appropriate treatment strategies that focus on compensatory techniques and adaptation methods for improved functioning and well-being.
Challenges around Using Agnosia in Mental Health Treatment
Limited awareness and recognition
A major challenge when it comes to using agnosia in mental health treatment is the limited awareness and recognition of this condition. Many healthcare professionals may not fully understand or recognise the symptoms of agnosia, which can lead to misdiagnosis or under treatment of individuals suffering from this perception impairment.
Difficulty in diagnosis
Diagnosing agnosia can be quite challenging due to its complex nature. The symptoms of agnosia can vary widely depending on the specific type, making it difficult for mental health professionals to identify and properly diagnose the condition. This lack of accurate diagnosis can hinder effective treatment planning and intervention strategies.
Impact on therapy outcomes
The presence of agnosia can significantly affect therapy outcomes for individuals with mental health conditions. It impairs their ability to accurately perceive and interpret sensory information, which may hinder their progress in therapy sessions.
This challenges therapists to adapt their approaches, modify techniques, or find alternative communication methods that cater to their patients’ impaired perception abilities.
Finally, agnosia is a condition that impairs a person's ability to recognize and interpret sensory information, such as objects, faces, sounds, colour, or smells. It is often caused by damage to specific areas of the brain, typically the occipital or temporal lobes. While the exact prevalence of agnosia is not known, it can occur in both children and adults, and can be acquired or congenital.
Living with agnosia requires individuals to develop coping strategies and adapt to a world that is often confusing and unpredictable. Although agnosia is a relatively rare condition, it is essential to increase awareness and understanding of its effects on individuals to foster empathy and support.
Within this article, we have explored different types of agnosia, the challenges faced by those living with this condition, and potential strategies for managing and navigating daily life with agnosia in health and disease.